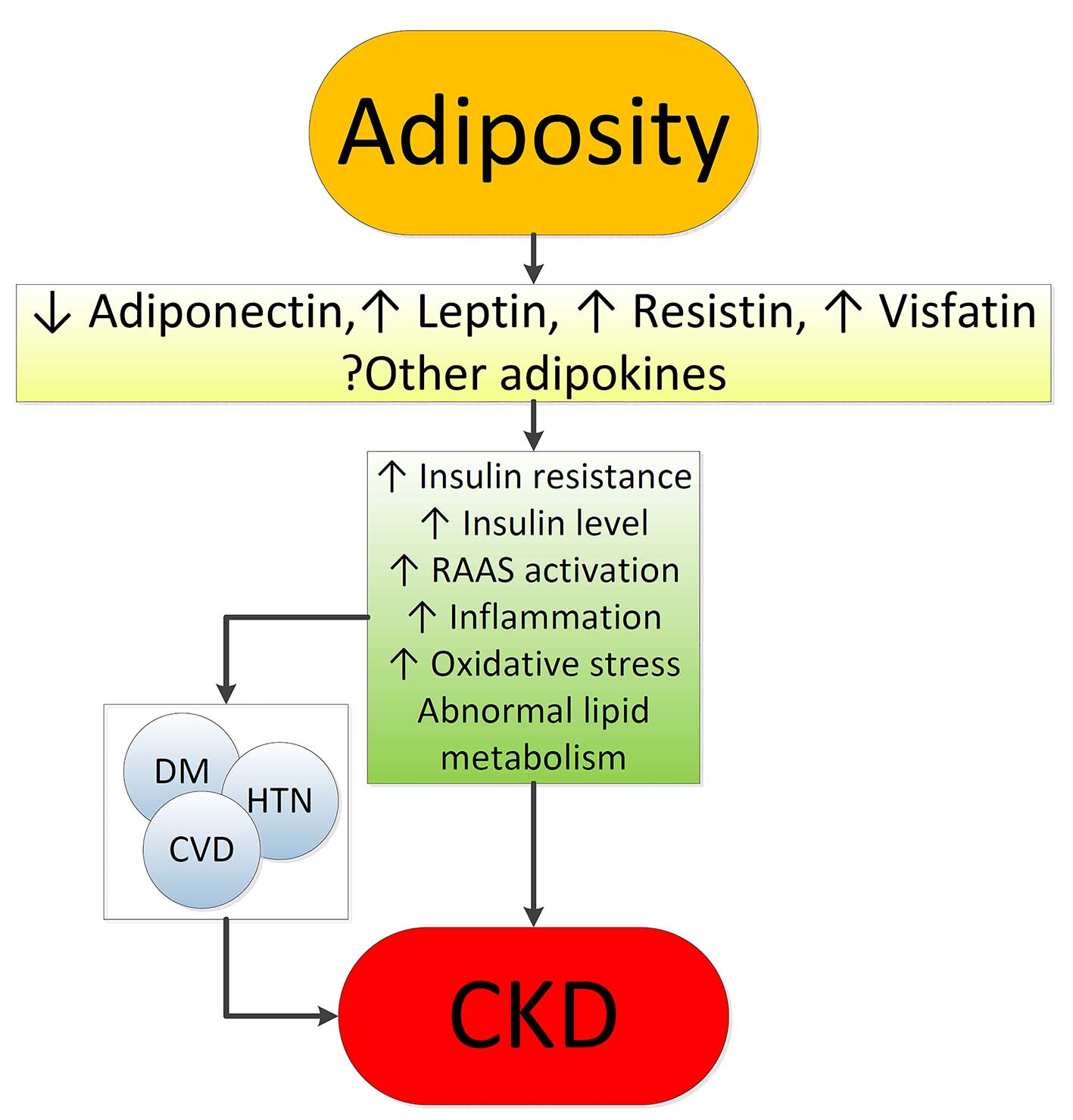
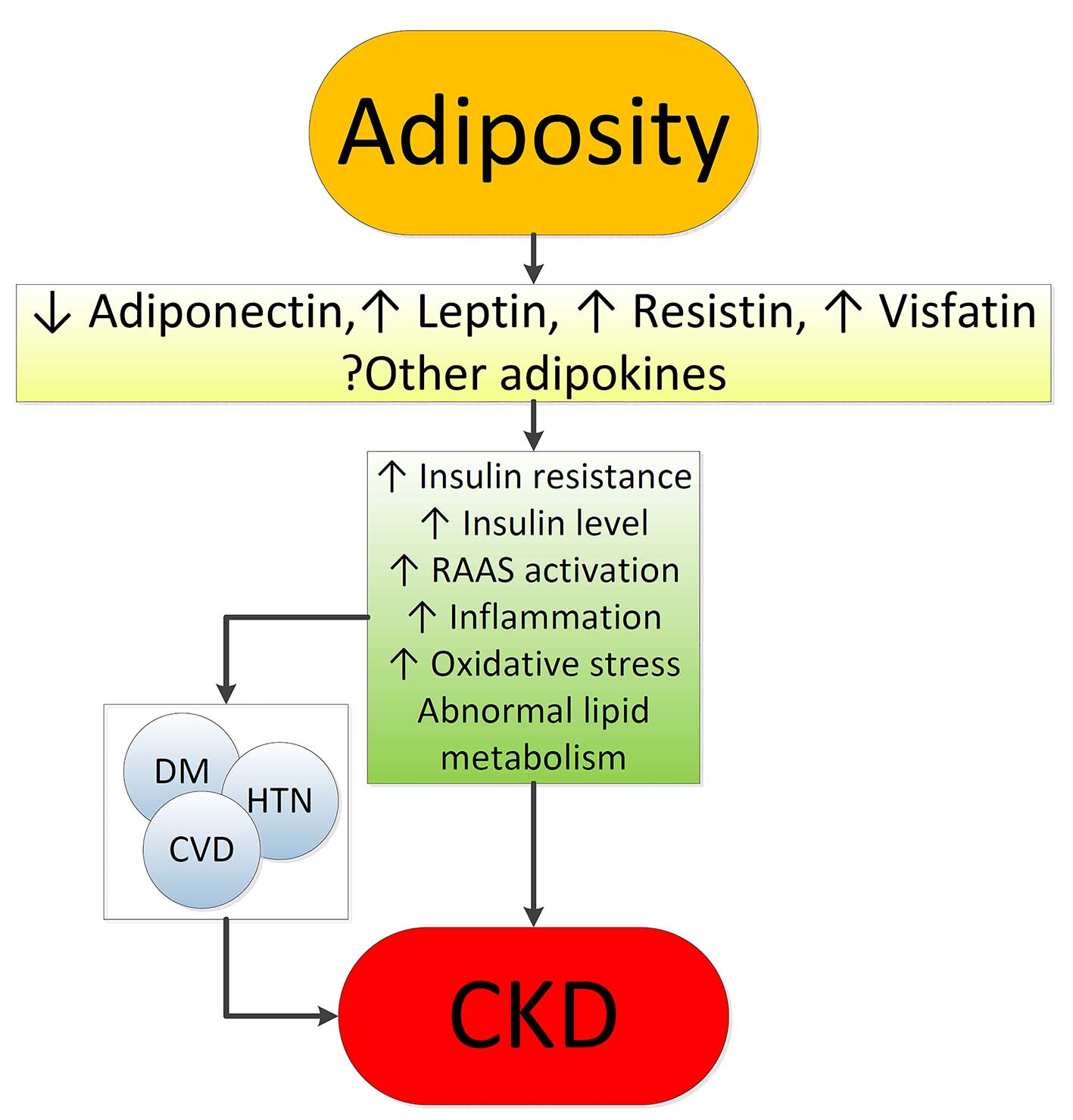
Figure 1. Putative mechanisms of action whereby obesity causes chronic kidney disease.
| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website http://www.wjnu.org |
Review
Volume 6, Number 1-2, June 2017, pages 1-9
Obesity and Kidney Disease: Hidden Consequences of the Epidemic
Figures
Table
| Study | Patients | Exposure | Outcomes | Results | Comments |
|---|---|---|---|---|---|
| *Normal weight: BMI 18.5 - 24.9 kg/m2; overweight: BMI 25.0 - 29.9 kg/m2; class I obesity: BMI 30.0 - 34.9 kg/m2; class II obesity: BMI 35.0 - 39.9 kg/m2; class III obesity: BMI ≥ 40 kg/m2. BMI: body mass index; CKD: chronic kidney disease; DM: diabetes mellitus; eGFR: estimated glomerular filtration rate; ESRD: end-stage renal disease; HR: hazard ratio; OR: odds ratio; UACR: urine albumin-creatinine ratio. | |||||
| Prevention of renal and vascular end-stage disease (PREVEND) study [8] | 7,676 Dutch individuals without diabetes | Elevated BMI (overweight and obese*), and central fat distribution (waist-hip ratio) | Presence of urine albumin 30 - 300 mg/24 h Elevated and diminished GFR | Obese + central fat: higher risk of albuminuria Obese ± central fat: higher risk of elevated GFR Central fat ± obesity associated with diminished filtration | Cross-sectional analysis |
| Multinational study of hypertensive outpatients [20] | 20,828 patients from 26 countries | BMI and waist circumference | Prevalence of albuminuria by dip stick | Higher waist circumference associated with albuminuria independent of BMI | Cross-sectional analysis |
| Framingham multi-detector computed tomography (MDCT) cohort [22] | 3,099 individuals | Visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) | Prevalence of UACR > 25 mg/g in women and > 17 mg/g in men | VAT associated with albuminuria in men, but not in women | Cross-sectional analysis |
| CARDIA (coronary artery risk development in young adults) study [11] | 2,354 community-dwelling individuals with normal kidney function aged 28 - 40 years | Obesity (BMI > 30 kg/m2) Diet and lifestyle-related factors | Incident microalbuminuria | Obesity (OR: 1.9) and unhealthy diet (OR: 2.0) associated with incident albuminuria | Low number of events |
| Hypertension detection and follow-up program [10] | 5,897 hypertensive adults | Overweight and obese BMI* vs. normal BMI | Incident CKD (1+ or greater proteinuria on urinalysis and/or an eGFR < 60 mL/min/1.73 m2) | Both overweight (OR: 1.21) and obesity (OR: 1.40) associated with incident CKD | Results unchanged after excluding diabetics |
| Framingham offspring study [9] | 2,676 individuals free of CKD stage 3 | High vs. normal BMI* | Incident CKD stage 3 Incident proteinuria | Higher BMI not associated with CKD3 after adjustments Higher BMI associated with increased odds of incident proteinuria | Predominantly white, limited geography |
| Physicians’ health study [13] | 11,104 initially healthy men in US | BMI quintiles Increase in BMI over time (vs. stable BMI) | Incident eGFR < 60 mL/min/1.73 m2 | Higher baseline BMI and increase in BMI over time both associated with higher risk of incident CKD | Exclusively men |
| Nation-wide US veterans administration cohort [14] | 3,376,187 US veterans with baseline eGFR ≥ 60 mL/min/1.73 m2 | BMI categories from < 20 to > 50 kg/m2 | Rapid decline in kidney function (negative eGFR slope of > 5 mL/min/1.73 m2) | BMI > 30 kg/m2 associated with rapid loss of kidney function | Associations more accentuated in older individuals |
| Nation-wide population-based study from Sweden [12] | 926 Swedes with moderate/advanced CKD compared to 998 controls | BMI ≥ 25 vs. < 25 kg/m2 | CKD vs. no CKD | Higher BMI associated with three times higher risk of CKD | Risk strongest in diabetics, but also significantly higher in non-diabetics Cross-sectional analysis |
| Nation-wide population based study in Israel [17] | 1,194,704 adolescent males and females examined for military service | Elevated BMI (overweight and obesity) vs. normal BMI* | Incident ESRD | Overweight (HR: 3.0) and obesity (HR: 6.89) associated with higher risk of ESRD | Associations strongest for diabetic ESRD, but also significantly higher for non-diabetic ESRD |
| The Nord-Trondelag health study (HUNT-1) [15] | 74,986 Norwegian adults | BMI categories* | Incidence of ESRD or renal death | BMI > 30 kg/m2 associated with worse outcomes | Associations not present in individuals with BL < 120/80 mm Hg |
| Community-based screening in Okinawa, Japan [16] | 100,753 individuals > 20 years old | BMI quartiles | Incidence of ESRD | Higher BMI associated with increased risk of ESRD in men, but not in women | Average BMI lower in Japan compared to Western countries |
| Nation-wide US veterans administration cohort [19] | 453,946 US veterans with baseline eGFR < 60 mL/min/1.73 m2 | BMI categories from < 20 to > 50 kg/m2 | Incidence of ESRD Doubling of serum creatinine Slopes of eGFR | Moderate and severe obesity associated with worse renal outcomes | Associations present but weaker in patients with more advanced CKD |
| Kaiser Permanente Northern California [18] | 320,252 adults with and without baseline CKD | Overweight, class I, II and extreme obesity vs. normal BMI* | Incidence of ESRD | Linearly higher risk of ESRD with higher BMI categories | Associations remained present after adjustment for DM, hypertension and baseline CKD |
| REGARDS (reasons for geographic and racial differences in stroke) study [21] | 30,239 individuals | Elevated waist circumference or BMI | Incidence of ESRD | BMI above normal not associated with ESRD after adjustment for waist circumference Higher waist circumference associated with ESRD | Association of waist circumference with ESRD became on-significant after adjustment for comorbidities and baseline eGFR and proteinuria |