| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website http://www.wjnu.org |
Case Report
Volume 3, Number 1, March 2014, pages 54-57
Cystoscopic Extraction of a Whole Pen From the Bladder: A Case Report and Review of Bladder Foreign Bodies’ Treatment Options
Ali Abdel Raheema, b, Khaled Hafeza, Ahmed Sherbinia, Ahmed Zoaira, Ahmed Eissaa
aUrology Department, Tanta University Hospital, Egypt
bCorresponding author: Ali Abdel Raheem, Endourology Unit, Urology Department, Tanta University Medical School, Egypt
Manuscript accepted for publication February 20, 2014
Short title: Cystoscopic Extraction of Foreign Bodies
doi: https://doi.org/10.14740/wjnu150w
| Abstract | ▴Top |
Foreign bodies (FBs) in the urinary bladder are relatively rare. FBs introduced through the urethra are the most common cause of bladder FBs and introduced for the purpose of sexual stimulation. Patients may be asymptomatic or presented with various lower urinary tract symptoms. Here we reported the management of a pen introduced inside the bladder of a young female patient.
Keywords: Pen; Foreign body; Bladder; Lithotrite
| Introduction | ▴Top |
Foreign bodies (FBs) in the urinary bladder are relatively rare. Various unusual bladder FBs were reported such as needle, bullet, fish hooks, metal rods, animal feather, hair pins, pieces of a candle, a thermometer, screws, pellets, wires, wooden sticks, pieces of fish, pencil, telephone cables, a gauze pack, a toothbrush, scalpel blade and fetal bone [1].
Bladder FBs may be self-inserted through the urethra, iatrogenic, migratory or due to penetrating trauma. FBs introduced through the urethra are the most common cause of bladder FBs. It is inserted for the purpose of eroticism and sexual stimulation or during intoxication. It may be also associated with psychiatric disorders or senility [2].
Patient with bladder FBs may be asymptomatic or complains of dysuria, hematuria, suprapubic pain, frequency, poor stream and urinary retention. Some complications may be associated with long standing bladder FBs as recurrent urinary tract infection and stone formation. Rarely some patients may develop serious complications such as perforation of the urinary bladder [3] or hydronephrosis [4] with impairment of renal function.
Here we reported the first successful endoscopic extraction of a whole self-inflected pen using mechanical lithotripter in a female patient.
| Case Report | ▴Top |
An 18-year-old female patient presented to our emergency department complaining of severe dysuria, hematuria and suprapubic pain which occurred after self-insertion of a pen inside the bladder during masturbation. Physical examination revealed suprapubic tenderness on palpation. Genital examination was normal and hymen was not ruptured. Laboratory findings were normal except urine analysis showed RBCs over 100. Ultrasound, X-ray pelvis and computed tomography confirmed the presence of a pen inside the bladder (Fig. 1A, B). Under general anesthesia, visualizing cystoscopy was performed and the pen was successfully extracted (Fig. 2, 3). The operative time was 35 min with no intraoperative complications. Twenty °F Foley’s catheter was inserted for 10 days to ensure complete healing of the minor bladder perforations. Her postoperative recovery was satisfactory.
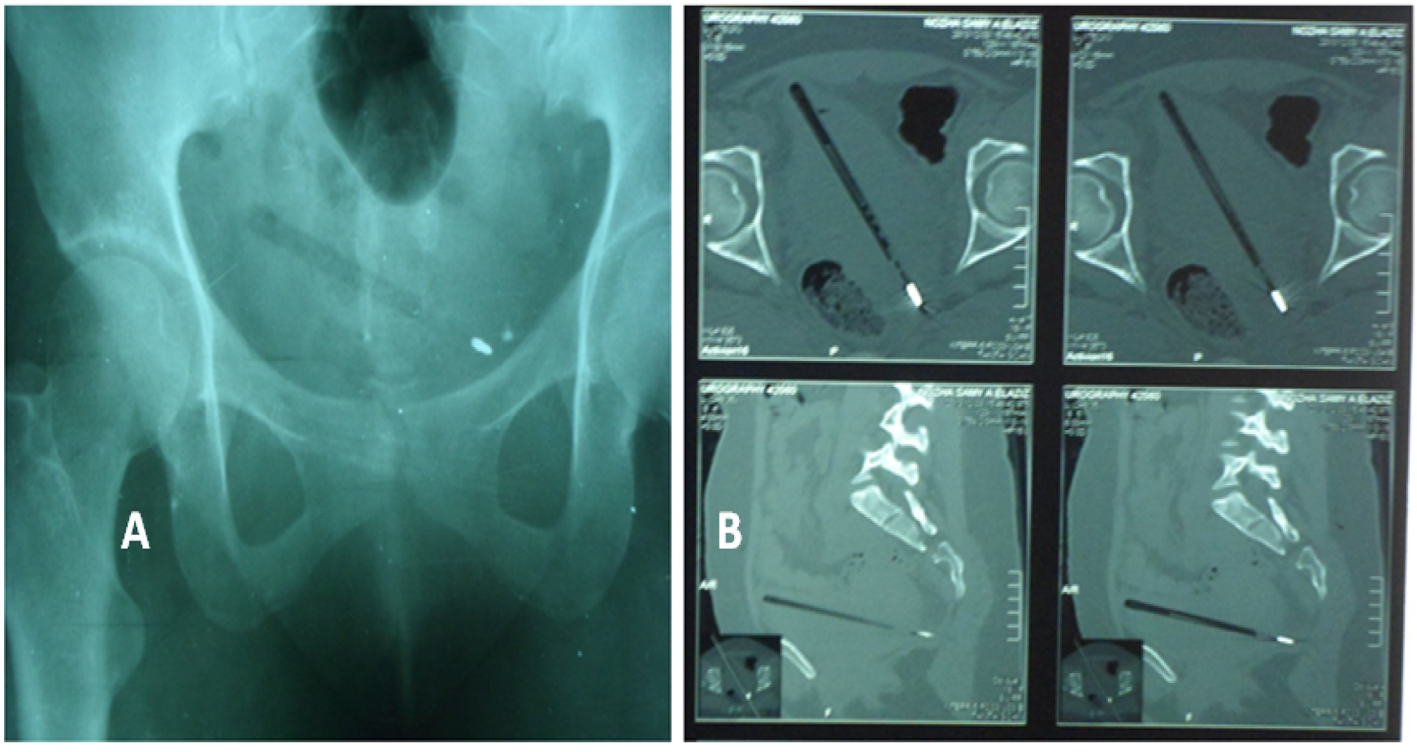 Click for large image | Figure 1. (A) Plain-X-ray showing the pen (radio-opaque shadow is the metal tip of the pen). (B) Computer tomography showing the pen is hanged inside the bladder. |
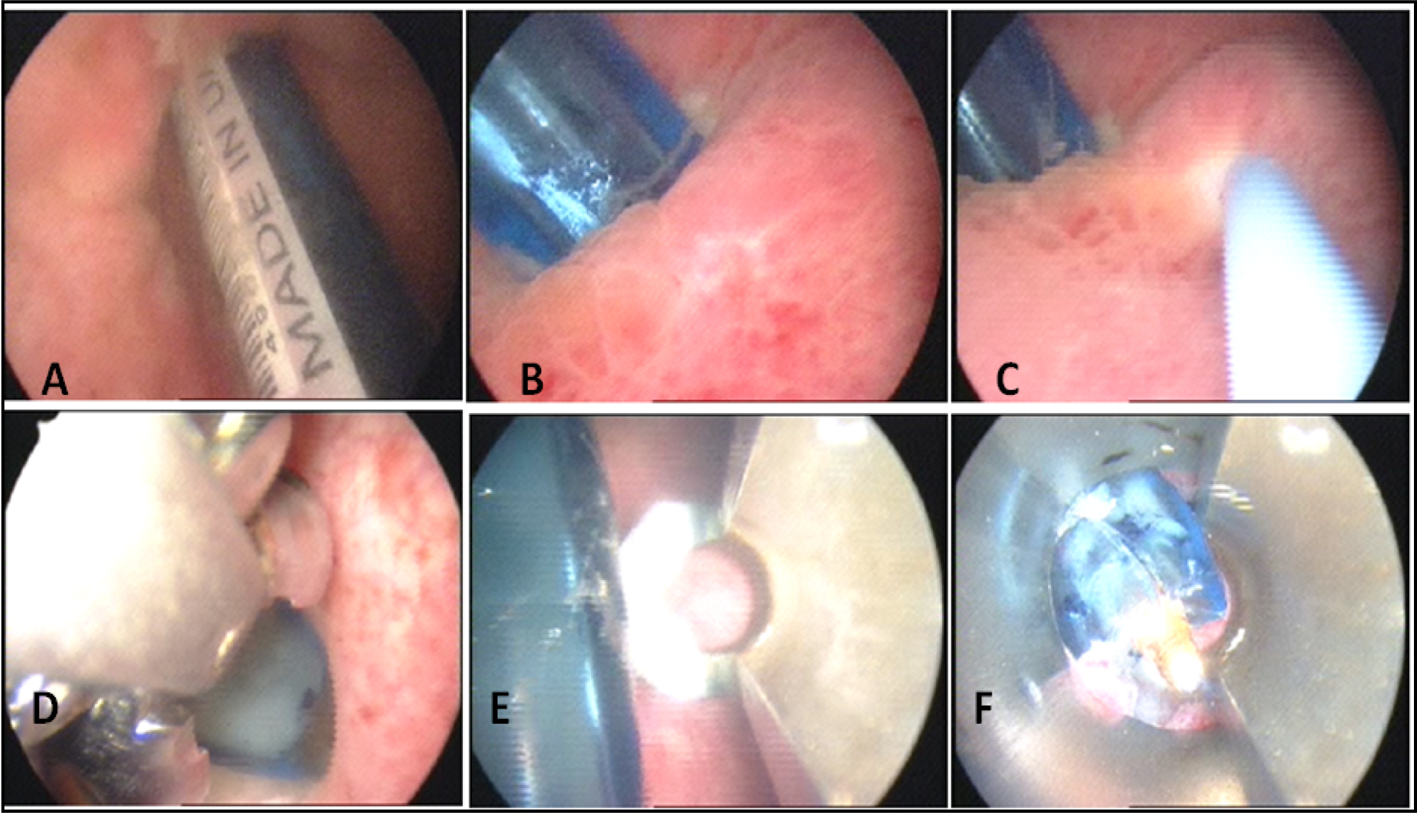 Click for large image | Figure 2. Steps of cystoscopic pen extraction: both pen ends penetrated into the bladder walls (A, B). The left ureter is secured (C). Failed trials of pen extraction using cold punch and forceps (D). Failed trials of pen fragmentation with the mechanical lithotripter as it was hard (E). Finally, we hold the tip of the pen with the lithotrite and disimpacted it backward away from the bladder mucosa, then pulled it with the lithotrite directed upward (F). |
 Click for large image | Figure 3. The whole pen after its extraction. |
| Discussion | ▴Top |
The presence of bladder FBs has always been an interesting topic representing a challenge of diagnosis and management to the urologist. Various treatment options are reported for the treatment of bladder FBs, for example, endoscopic, laparoscopic, percutaneous, radiological and open surgery. In some cases, a combination of techniques is required; however, still endoscopic retrieval is the preferred treatment among urologists. The method of choice for extraction varies according to the size and mobility of the object inside the bladder [1]. In addition, the availability of surgical instrumentations and urologist experience plays an important role.
The increased use of minimally invasive endoscopy for treatment of urinary stones has also provided different grasping tools amenable for extracting different bladder FBs. A wide range of grasping instruments may be required including stone basket [5, 6], grasping forceps [7], stone punch, snares and other modified instruments [8, 9]. Satisfactory success rate for cystoscopic extraction of bladder FBs was reported in literature ranging between 50 and 94% [7-9].
The presence of a pen in the urinary bladder is extremely rare and most cases are treated by surgical exploration as this may be due to its long length with increased liability to perforate owing to its sharp tip [10], or the formation of a large bladder stone over a neglected pen cap that requires open cystolithotomy [11]. However, endoscopy was successfully used in the extraction of a piece of pen [12] and fragmentation of a stone encrusted around a pen cover [13]. Our case is a unique one as it is the first reported successful extraction of a whole pen from the bladder using a mechanical lithotripter “lithotrite”. Badenoch and Campbell (1937) reported a trial to remove a leather bootlace using lithotrite but they failed and shifted to open surgery [14]. We were faced by many difficulties during the procedures: 1) both ends of the pen were penetrating into the bladder wall, 2) the wide diameter of the pen which made it very difficult to hold by the ordinary grasping instruments and 3) the long length of the pen increased the risk of bladder wall perforation as we try to disimpact it from one side. Our main aim during pen extraction was to complete the procedure endoscopically without the need to shift to open surgery and we succeeded.
Bladder FBs treatment options
To minimize the hazards of open surgery and to maintain the minimally invasive advantages of endoscopy, many studies reported innovative trials and new techniques for bladder FBs removal. Ureteral catheters could be used to snare FBs, a resectocope has been used to extract a thermometer, while screws and sharp, pointed objects were extracted by a Blu-Tack nephroscope [15]. Younesi et al (2004) managed to remove a lidocaine carpule from the bladder using a nephroscope through a suprapubic percutaneous approach [16]. Moreover, holmium laser was reported to fragment and remove bladder FBs [17, 18].
In some patients, the extraction of FB from the bladder may be difficult and open surgery is indicated. To minimize the risk of open surgery, urologists innovated other techniques for treatment. Delair et al (2006) utilized a small suprapubic cystostomy (3 cm in length) to extract a toy frog guided by endoscopic visualization [19]. Other surgeons combined two techniques: percutaneous or laparoscopic technique with endoscopy to avoid open suprabubic cystostomy. Hutton and Huddart (1999) used percutaneous puncture for retrieval of an intravesical FB using direct transurethral visualization [20]. Moreover, a self-inflicted wire extending from the external meatus to the bladder was removed using combined rigid cystoscopy and suprapubic forceps [21]. Bukowski and Williams (1997) used a combined laparoscopic/endoscopic procedure to extract a migrated intraurethral stent from after distal hypospadias repair [22].
The role of laparoscopy in the treatment of bladder FBs has also been discussed. Feliu et al (2011) reported laparoscopic management of calcified bladder FB due to displaced tack after laparoscopic incisional hernia repair. Tacks were removed laparoscopically together with partial cystectomy [23]. Recently an encrusted polypropylene mesh could be extracted successfully from the bladder mucosa using single port laparoscopic surgery [24].
Also, a novel radiological technique was described using fluoroscope under local anesthesia to guide a gooseneck snare through endoscopic sheath to retrieve an FB after pushing it into the bladder [25].
In some cases, open surgery is indicated in sharp or large sized FB or after failed endoscopy [26, 27].
In conclusion, endoscopic retrieval of FBs has always been a challenge and quite satisfying procedure if done properly. It is now clear to us that the majority of bladder FBs can be treated successfully by endoscopy; however, open surgery still has a role if failed endoscopy, with large sized FB, migrating or solid impacted FBs. Also open surgery is indicated if endoscopic equipments are not available or lack of surgeon’s experience with endoscopic maneuvers.
Conflict of Interest
No conflict of interest.
Author Disclosure
No competing financial interests exist.
| References | ▴Top |
- van Ophoven A, deKernion JB. Clinical management of foreign bodies of the genitourinary tract. J Urol. 2000;164(2):274-287.
doi - Rosenthal M, Berkman P, Shapira A, Gil I, Abramovitz J. Urethral masturbation and sexual disinhibition in dementia: a case report. Isr J Psychiatry Relat Sci. 2003;40(1):67-72.
pubmed - Bantis A, Sountoulides P, Kalaitzis C, Giannakopoulos S, Agelonidou E, Foutzitzi S, Touloupidis S. Perforation of the urinary bladder caused by transurethral insertion of a pencil for the purpose of masturbation in a 29-year-old female. Case Rep Med. 2010;2010.
- Cho BS, Park KS, Kang MH, Han GS, Lee SY, Cha SH, Kim SJ. Unilateral hydronephrosis and hydroureter by foreign body in urinary bladder: a case report. J Korean Med Sci. 2012;27(6):704-706.
doi pubmed - Rahman NU, Elliott SP, McAninch JW. Self-inflicted male urethral foreign body insertion: endoscopic management and complications. BJU Int. 2004;94(7):1051-1053.
doi pubmed - Gonzalgo ML, Chan DY. Endoscopic basket extraction of a urethral foreign body. Urology. 2003;62(2):352.
doi - Malik MA, Ghaffar-Rehan A, Javed SH, Iqbal Z. Endoscopic Management of Foreign Body in Urethra and Urinary Bladder. Int J Nephrol Urol, 2009; 1(1):56-60.
- Mannan A, Anwar S, Qayyum A, Tasneem RA. Foreign bodies in the urinary bladder and their management: a Pakistani experience. Singapore Med J. 2011;52(1):24-28.
pubmed - Zeinali S, Mohammad Eram S, Azimifar SB, Lotfi V, Foulady P, Masrouri M. First report on the co-inheritance of (beta) IVS I-1 (G—>T) Thalassemia with the (gamma) CD85 [Phe—>Ser (F1) (TTT—>TCT)] HbA2 Etolia in Iran. Haematologica. 2006;91(6 Suppl):ECR15.
pubmed - Cury J, Coelho RF, Srougi M. Retroperitoneal migration of a self-inflicted ballpoint pen via the urethra. Int Braz J Urol. 2006;32(2):193-195.
doi pubmed - Mondaini N, Bartoletti R. Images in clinical medicine. Intravesical foreign body. N Engl J Med. 2007;357(6):588.
doi pubmed - Ersoy H, Saonak L, Topaloolu H, BakyrtapH, pahin E, Kiper A. An extremely rare foreign material in the bladder: a piece of pen. Gulhane Typ Dergisi 2007;49:181-182.
- Sharma UK, Rauniyar D, Shah WF. Intravesical foreign body: case report. Kathmandu Univ Med J (KUMJ). 2006;4(3):342-344.
- Badenoch W, Campbell RI. Foreign bodies in the urinary bladder with a report of two cases. British journal of surgery. 1937;25:133-138.
doi - Georgius P. A novel method to remove an unusual intravesical foreign body (Blu-Tack). BJU Int. 2000;86(6):749-750.
doi pubmed - Younesi M, Ahmadnia H, M ASLZ. An unusual foreign body in the bladder and percutaneous removal. Urol J. 2004;1(2):126-127.
pubmed - Wyatt J, Hammontree LN. Use of Holmium:YAG laser to facilitate removal of intravesical foreign bodies. J Endourol. 2006;20(9):672-674.
doi pubmed - Habermacher G, Nadler RB. Intravesical holmium laser fragmentation and removal of detached resectoscope sheath tip. J Urol. 2005;174(4 Pt 1):1296-1297.
doi pubmed - DeLair SM, Bernal RM, Keegan KA, Ellison LM. Ship in a bottle: rapid extraction of large intravesical foreign bodies. Urology. 2006;67(3):612-613.
doi pubmed - Hutton KA, Huddart SN. Percutaneous retrieval of an intravesical foreign body using direct transurethral visualization: a technique applicable to small children. BJU Int. 1999;83(3):337-338.
doi pubmed - Sawyer MD, Proano JM, Spirnak JP. Removal of retained Foley catheter in bladder with novel use of ureteral catheter: lasso technique. Urology. 2008;71(5):962-963.
doi pubmed - Moslemi MK, Sorani M. Self-inflicted male bladder foreign body: its endoscopic removal using a rigid cystoscope and a suprapubic forceps. Case Rep Urol. 2013;2013:729013.
- Bukowski TP, Williams CR. Percutaneous intravesical retrieval of a misplaced urethral stent: new laparoscopic instrumentation. J Urol. 1997;157(6):2257.
doi - Feliu X, Claveria R, Besora P, Luque D, Vinas X. A calcified foreign body in the bladder due to : an unusual complication after laparoscopic incisional hernia repair. Surg Laparosc Endosc Percutan Tech. 2011;21(1):e28-30.
doi pubmed - Ingber MS, Stein RJ, Rackley RR, Firoozi F, Irwin BH, Kaouk JH, Desai MM. Single-port transvesical excision of foreign body in the bladder. Urology. 2009;74(6):1347-1350.
doi pubmed - Seong BJ, Kim SJ, Kim HS, Kim DY, Chung JM, Choi S. Acute urinary retention due to urethral foreign bodies. J Korean Continence Soc. 2006;10:60-62.
- Percutaneous Removal of a Very Unusual Foreign Body from the Bladder: Case Report and Literature Review Taylan Oksay, Alper Ozorak, Osman Ergun, Mustafa BurakHoscan, AlimKosar, Tekin Ahmet Serel, JAEM. 2013;12:231-233.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
