| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website http://www.wjnu.org |
Case Report
Volume 4, Number 4, December 2015, pages 267-269
Reninoma: A Case Report
Bibiana Lopez-Lopeza, Maria Juana Perez-Lopeza, Valencia-de Leon Bettina Fabiolab, Rosario Mora-Camposc, Felix Santaella-Torresd, Daniel Salazar-Exairee, f
aDepartamento de Nefrologia, Centro Medico Nacional La Raza IMSS, Mexico
bEscuela de Medicina, “Universidad Justo Sierra”, Mexico
cDepartamento de Patologia Clinica, Centro Medico Nacional La Raza IMSS, Mexico
dDepartamento de Urologia, Centro Medico Nacional La Raza IMSS, Mexico
eUnidad de Investigacion en Epidemiologia Clinica, Centro Medico Nacional La Raza, IMSS, Mexico, D.F., Mexico
fCorresponding Author: Daniel Salazar-Exaire, Unidad de Investigacion en Epidemiologia Clinica, Centro Medico Nacional La Raza, IMSS, Mexico, D.F., Mexico
Manuscript accepted for publication November 10, 2015
Short title: Reninoma
doi: http://dx.doi.org/10.14740/wjnu243w
| Abstract | ▴Top |
Reninoma is a tumor of the renal juxtaglomerular cell apparatus that causes hypertension and hypokalemia via hypersecretion of renin. We describe a case of reninoma. Imaging studies revealed the presence of a lesion in the renal cortex, which, on immunohistochemistry, was identified as a juxtaglomerular cell tumor. Following nephrectomy, the blood pressure and hypokalemia were normalized.
Keywords: Juxtaglomerular cell tumor; Reninoma; Hypertension; Hyperaldosteronism
| Introduction | ▴Top |
Juxtaglomerular cell tumor (JGCT) is a rare cause of secondary hypertension manifested by hypertension, hypokalemia and elevated serum renin, symptoms that are potentially surgically curable. JGCT or reninoma is an infrequent cause of secondary hypertension. Since the first case described by Robertson et al in 1967 [1], there have been about 100 cases reported. However, this tumor is underdiagnosed due to the lack of clinical suspicion and because it may have an irregular presentation. This classification is based on the behavior of serum potassium and hypertension, although metabolic alkalosis and hyperaldosteronism are not always constant and are not taken into account for classification.
| Case Report | ▴Top |
We present the case of a 19-year-old female without a family history of hypertension. She had generalized headache 7 months prior to her admission. Physical examination was positive for hypertension (170/120) and asymptomatic hypokalemia (2.6 mEq/L). She had preserved renal function with creatinine of 0.57 mg/dL, normal urinalysis, sodium of 138 mEq/L, serum potassium of 2.6 mEq/L, Cl of 108 mEq/L, 24-h urine electrolytes of potassium of 57.96 mmol, sodium of 115.20 mmol, chloride of 88.2 mmol, and normal metanephrines. She demonstrated a negative immune profile, cortisol of 10 μg/dL (5 - 25 morning, 2.5 - 12.5 afternoon), aldosterone of 95 pg/mL (supine 10 - 160, standing 40 - 310), renin of 294.4 μUL/mL (supine 2.8 - 39.9, standing 4.4 - 46.1) with balanced metabolic alkalosis (pH 7.40, pCO2 46, HCO3 27.9). Abdominal computed tomography (CT) reported preserved kidney size with a hypodense image in the cortex of the mid-region of the right kidney of 20.9 × 14.5 mm, which was not contrast enhanced (Fig. 1). The patient underwent right laparoscopic tumor removal with a definitive pathological diagnosis with positive immunohistochemistry for CD117 and actin (Fig. 2, 3), respectively, and negative for cytokeratin, desmin, S-100 protein and chromogranin. At the time we did not have CD34 marker but, based on the clinical, biochemical and imaging behavior, diagnosis JGCT was made. On the day following surgery, the patient did not require continuation of antihypertensives. Serum potassium returned to normal levels and metabolic alkalosis resolved.
 Click for large image | Figure 1. Contrast tomography of the abdomen that reports preserved kidney size with a hypodense image in the cortical region of the right kidney of 20.9 × 14.5 mm that is not reinforced with contrast. |
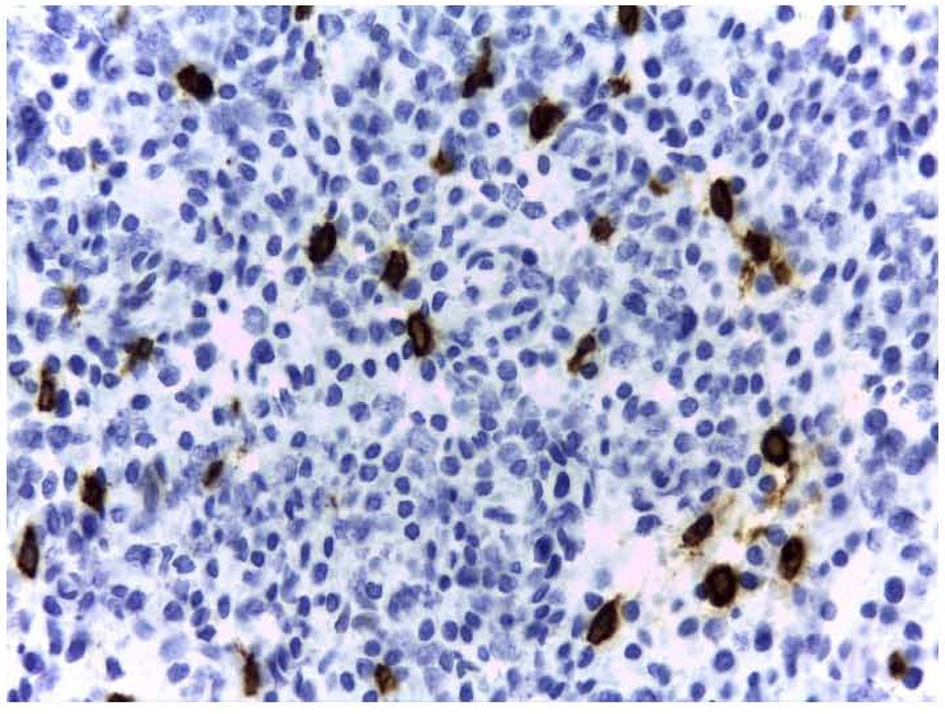 Click for large image | Figure 2. Optical microscopy of a histological section of the removed tumor and stained with peroxidase-conjugated anti-CD117 antibodies (original magnification, × 40). |
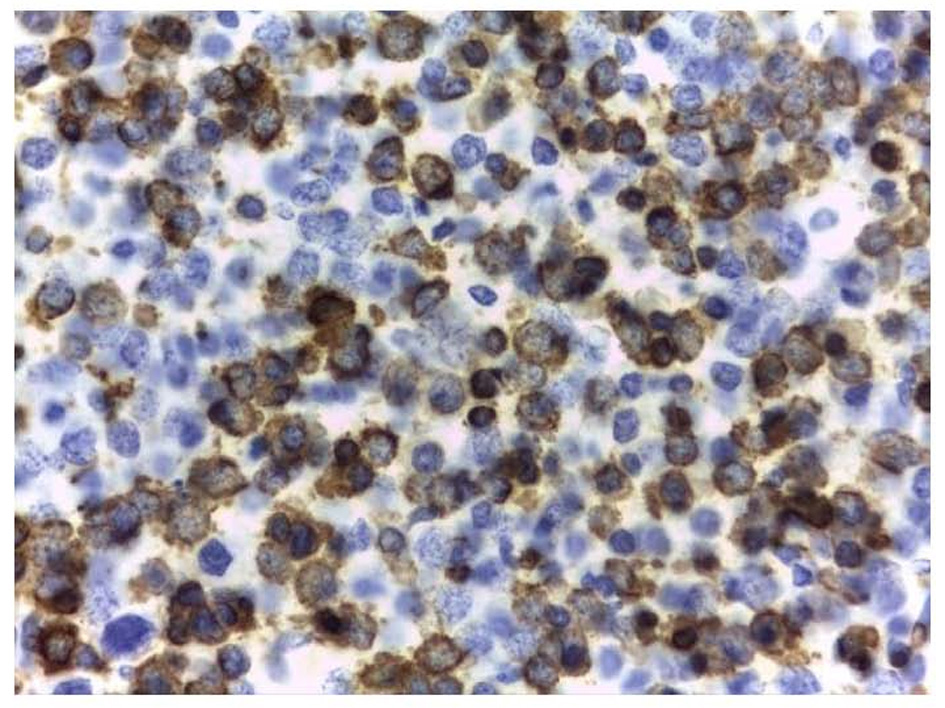 Click for large image | Figure 3. Optical microscopy of a histological section of the removed tumor and stained with peroxidase-conjugated anti-actin antibodies (original magnification, × 40). |
| Discussion | ▴Top |
JGCT is believed to be a benign tumor, although in 2004 Duan et al reported a metastatic reninoma [2]. Although it was not until 1968 that Kihara et al gave it the name for which it is presently known [3]. It has a peak incidence between the second and third decades of life, with a female predominance (2:1). The most frequent clinical presentation is the classic triad of hypertension, hypokalemia and renin or high renin activity [4].
Renal ultrasound shows a hypoechoic mass; however, it is useful to make a differential diagnosis especially in malignant lesions. CT is therefore recommended where those malignant lesions acquire an important enhancement. On tomography, reninoma appears as a well-circumscribed hypodense cortical mass that does not enhance in the arterial phase despite its profuse vascularity. This is probably due to the vasoconstriction induced by the renin. Without a doubt, definitive diagnosis is made immunohistochemically and the clinical behavior on tumor resection, although 10% of patients may persist with hypertension due to angiopathic damage [4].
During light microscopy, polygonal cells with eosinophilic cytoplasm and nucleolus located at the center are observed but these characteristics are variable; therefore, immunohistochemistry is carried out to make the differential diagnosis. Reninoma is (+) for actin, CD34 and CD117, negative for cytokeratin, desmin, protein S-100, HMB-45, chromogranin and synaptophysin [5]. Using electron microscopy, a search is made for intracytoplasmic granules, renin reservoirs that can be detected by Bowie staining and periodic acid-Schiff. The positivity of renin in the cytoplasm confirms the diagnosis, but it can also be positive in Wilms tumor, clear cell carcinomas and oncocytomas [5].
In conclusion, JGCT is a cause of potentially curable arterial hypertension. It should be considered in the presence of difficult-to-control hypertension especially in young adults so as to not overlook carrying out a comprehensive study protocol.
Primary reninoma was first described as a cause of hypertension and hypokalemia in 1967 [1]. It is rare, with an estimated incidence of about 1 of 5,000 hypertensive patients, an average duration of hypertension of > 5 years prior to diagnosis, and a mild female preponderance. The diagnosis has usually been made preoperatively by a combination of 1) biochemical measures, particularly hypokalemia and demonstration of excess renin secretion from the affected kidney, and 2) imaging, usually CT or MRI scan localization of a relatively avascular, well-circumscribed lesion. Confirmation has involved description of the typical encapsulated tumor, with histologic features including clusters of polygonal cells with positive renin staining, the presence of endocrine and vascular smooth muscle cells, and transitional cells containing prominent secretory granules, myofilaments, and attachment bodies. In all previous reports, a tumor has been visible on imaging prior to surgery. While earlier reports described nephrectomy as standard therapy, improvement in preoperative localization procedures has allowed the development of renal-sparing, minimally invasive surgery [6, 7] and electrolyte control was satisfactory in our patient with medical therapy. However, a laparoscopic approach allowed minimal morbidity associated with nephrectomy, her blood pressure subsequently returned to normal thus blood pressure and the procedure was curative.
Conflict of Interest
None.
Grant Support
This case report is supported by grant (2005/1/I/178) from FIS Mexico.
| References | ▴Top |
- Robertson PW, Klidjian A, Harding LK, Walters G, Lee MR, Robb-Smith AH. Hypertension due to a renin-secreting renal tumour. Am J Med. 1967;43(6):963-976.
doi - Duan X, Bruneval P, Hammadeh R, Fresco R, Eble JN, Clark JI, Vigneswaran WT, et al. Metastatic juxtaglomerular cell tumor in a 52-year-old man. Am J Surg Pathol. 2004;28(8):1098-1102.
doi pubmed - Kihara I, Kitamura S, Hoshino T, Seida H, Watanabe T. A hitherto unreported vascular tumor of the kidney: a proposal of "juxtaglomerular cell tumor". Acta Pathol Jpn. 1968;18(2):197-206.
doi - Venkateswaran R, Hamide A, Dorairajan LN, Basu D. Reninoma: a rare cause of curable hypertension. BMJ Case Rep. 2013;2013
- Kuroda N, Gotoda H, Ohe C, Mikami S, Inoue K, Nagashima Y, Petersson F, et al. Review of juxtaglomerular cell tumor with focus on pathobiological aspect. Diagn Pathol. 2011;6:80.
doi pubmed - Kashiwabara H, Inaba M, Itabashi A, Ishii J, Katayama S. A case of renin-producing juxtaglomerular tumor: effect of ACE inhibitor or angiotensin II receptor antagonist. Blood Press. 1997;6(3):147-153.
doi pubmed - Mete UK, Niranjan J, Kusum J, Rajesh LS, Goswami AK, Sharma SK. Reninoma treated with nephron-sparing surgery. Urology. 2003;61(6):1259.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
