| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website http://www.wjnu.org |
Case Report
Volume 5, Number 3, September 2016, pages 63-66
Two Cases of Acute Focal Bacterial Nephritis
Ryosuke Shibataa, Nobuhiro Takeuchib, c, Masanori Takadaa, Akihito Otsukaa
aDepartment of Internal Medicine, Kawasaki Hospital, 3-3-1 Higashiyama-cho, Hyogo-ku, Kobe-shi, Hyogo 652-0042, Japan
bDepartment of Internal Medicine, Kobe Tokushukai Hospital, 1-3-10 Kamitakamaru, Tarumi-ku, Kobe-shi, Hyogo 655-0017, Japan
cCorresponding Author: Nobuhiro Takeuchi, Department of Internal Medicine, Kobe Tokushukai Hospital, 1-3-10 Kamitakamaru, Tarumi-Ku, Kobe-shi, Hyogo, 655-0017, Japan
Manuscript accepted for publication September 13, 2016
Short title: Acute Focal Bacterial Nephritis
doi: http://dx.doi.org/10.14740/wjnu280w
| Abstract | ▴Top |
Acute focal bacterial nephritis (AFBN) is a bacterial infection of the renal parenchyma without abscess formation and is classified as a subtype of acute renal pyelitis. There are many reports of AFBN in pediatrics; however, urinary tract infection, cystitis, or pyelitis developed into AFBN in few adult cases. AFBN symptoms include fever, shivering, back pain, and/or costovertebral angle tenderness. Here, we report two adult cases of AFBN in which its diagnosis using contrast-enhanced computed tomography was helpful.
Keywords: Acute focal bacterial nephritis; Renal pyelitis; Contrast-enhanced computed tomography
| Introduction | ▴Top |
Acute focal bacterial nephritis (AFBN), sometimes called as acute lobar nephronia, is an acute, localized non-liquefactive bacterial infection of the kidney [1]. Although there are many reports of AFBN in pediatrics caused by congenital urinary malformation or vesicoureteral reflex (VUR), lesser attention for this condition is drawn in adults than in children. AFBN can be diagnosed by characteristic findings on contrast computed tomography (CT) scans. Typically, AFBN yields high negative blood culture and low positive urine culture results; therefore, it is difficult to diagnose AFBN without contrast-enhanced CT. Here, we present two adult cases of AFBN, which lacked the typical clinical presentation.
| Case Reports | ▴Top |
Case 1
A 41-year-old female visited a home clinic complaining of high grade fever (38.5 °C) and a severe headache which lasted for a couple of days. Meningitis was suspected from her medical consultation and physical examination. Following that, she was referred to our emergency department for further examination. Her past medical history included diabetes milieus type II, which was treated using oral drugs. Physical examination upon arrival revealed that her blood pressure was 140/80 mm Hg, heart rate was 86 beats/min with regular rhythm, blood oxygen saturation was 100% under atmospheric conditions, and body temperature was 36.0 °C. Blood chemistry analyses revealed severe inflammation (12,900/μL white blood cells (WBCs)/μL with 83.3% neutrophils and 39.2 mg/dL C-reactive protein), mild hyponatremia (131 mEq/mL), coagulant dysfunction (103% prothrombin, 39.0 s activated partial thromboplastic time, 1,014 mg/dL fibrinogen, and 3.7 μg/mL D-dimer), and impaired glucose tolerance (231 mg/dL glucose and 8.0% hemoglobin A1c). Further, mildly decreased albumin (3.7 g/dL), and mildly increased total bilirubin (1.7 mg/dL), gamma-glutamyltransferase (211 IU/L), alkaline phosphatase (469 IU/L), and lactate dehydrogenase (355 IU/L) were also revealed. Although she suffered intolerable head pain with queasiness, physical examination revealed no neck stiffness, Kernig, or Brudzinski sign, or costovertebral angle tenderness. Electrocardiography revealed a normal, regular heart rhythm without ST changes. Brain and chest CT revealed nothing that suggested infected lesions. Cerebrospinal fluid (CSF) culture and urine culture detected no bacteria, but blood culture revealed the presence of Escherichia coli (Fig. 1a). Urinalysis revealed 1 - 4 WBCs per high-power field (HPF) and 5 - 9 red blood cells (RBCs)/HPF with no bacteria. Non-contrast CT revealed mildly swollen right kidney accompanied by fat stranding in the peritoneal cavity, which suggested inflammation (Fig. 1b). Then contrast-enhanced CT was performed on the day of admission, revealing wedge-shaped, non-contrast, and low density mass-like lesions in the right kidney consistent with AFBN (Fig. 1c). Consequently, anti-bacterial agents were initiated (Fig. 2). After 3 weeks of antibacterial treatment, chemical analyses of inflammatory response dramatically improved, and symptoms completely disappeared.
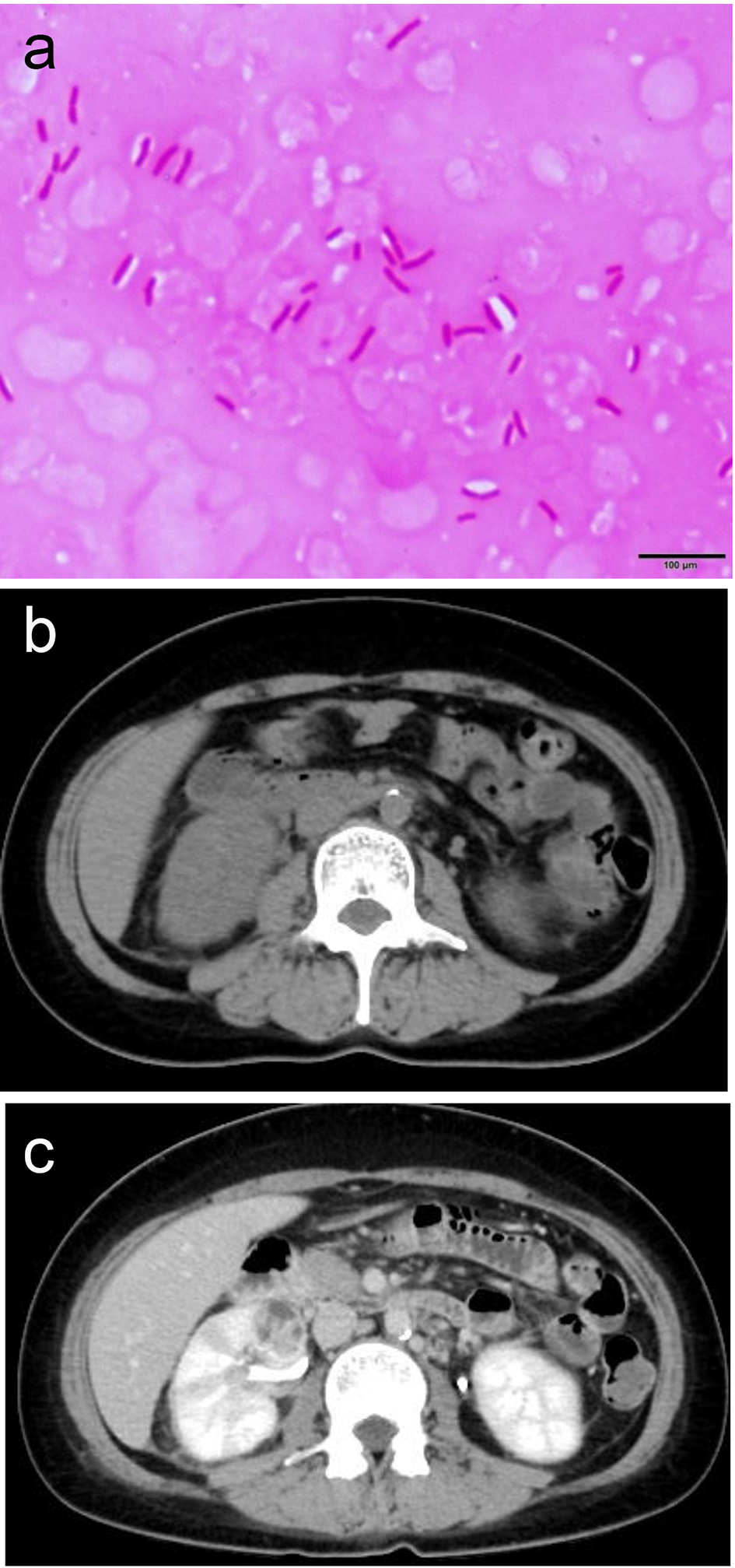 Click for large image | Figure 1. (a) E. coli was revealed by blood culture. (b) Mildly swollen right kidney accompanied by fat stranding in the peritoneal cavity suggesting inflammation. (c) Wedge-shaped, non-contrast, and low density mass-like lesions in the right kidney consistent with AFBN. |
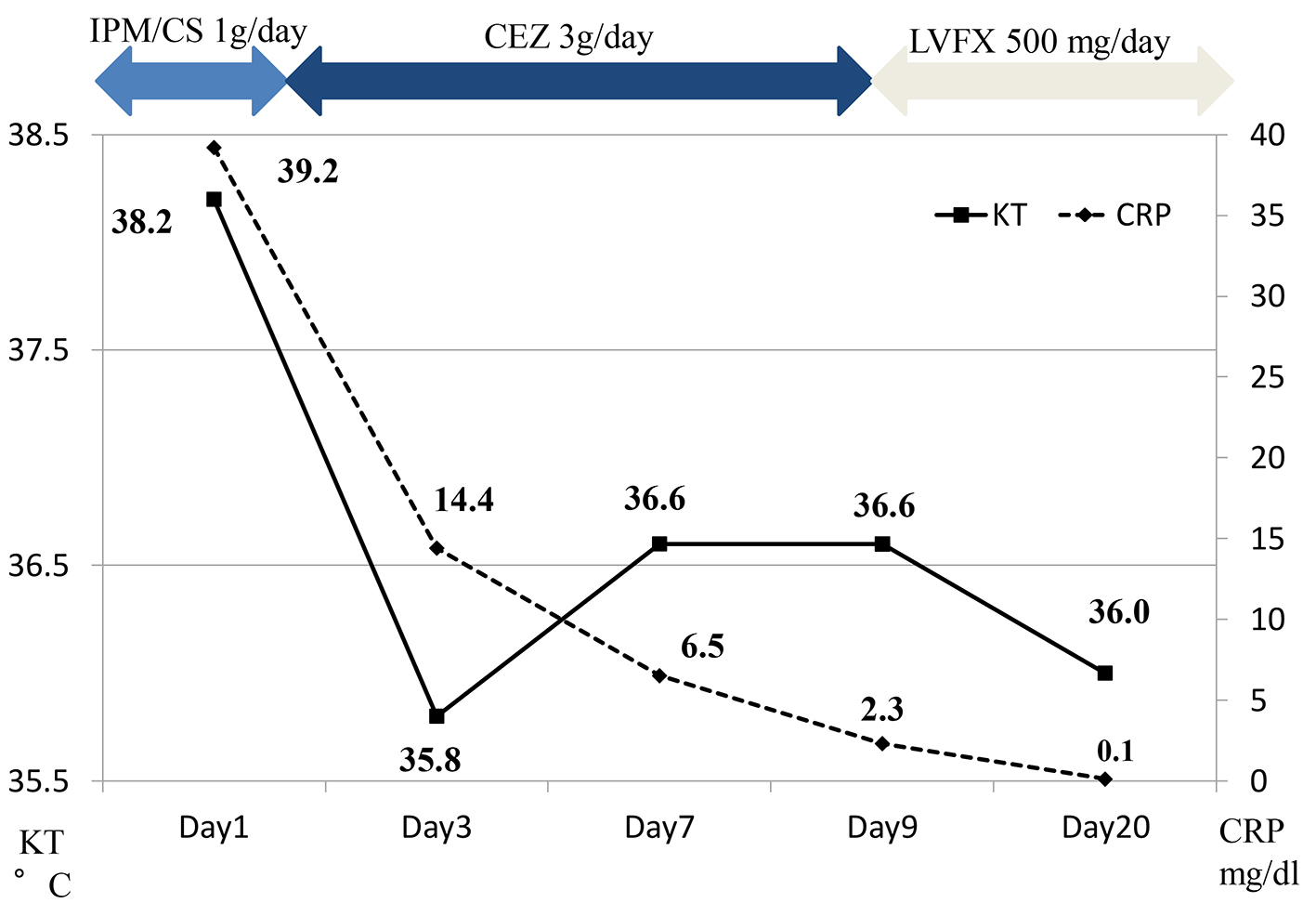 Click for large image | Figure 2. Clinical course of the case 1. IPM/CS: imipenem/cilastatin; CEZ: cefazolin; LVFX: levofloxacin. |
Case 2
A 78-year-old female presented to our hospital with complaints of fatigue, headache, and low grade fever lasting for a couple of days. Her medical history included hypertension, which was treated using medicine. She had no history of urinary tract infection. Upon arrival, her blood pressure was 133/78 mm Hg, heart rate was 76 beats/min with regular rhythm, blood oxygen saturation was 99% under atmospheric conditions, and body temperature was 37.2 °C. Blood chemistry analyses revealed severe inflammation (18,500 WBCs/μL with 79.8% neutrophils and 22.0 mg/dL C-reactive protein), coagulant dysfunction (72% prothrombin, 45.5 s activated partial thromboplastic time, 1,014 mg/dL fibrinogen, and 1.5 μg/mL D-dimer), and unimpaired glucose tolerance (110 mg/dL glucose and 5.9% hemoglobin A1c). Further, mildly decreased albumin (3.3 g/dL), mildly increased total bilirubin (1.5 mg/dL), 160 IU/L γ-glutamyltransferase, 702 IU/L alkaline phosphatase, and 354 IU/L lactate dehydrogenase were also revealed. Chest radiography revealed no shadows indicative of pneumonia. Urinalysis revealed 1 - 4 WBCs/HPF and 5 - 9 RBCs/HPF with no bacteria. Urinary and blood culture were negative for bacteria. Although she had no abdominal symptoms, non-contrast, whole-body CT was performed to further explore the possibility of infection. Non-contrast CT revealed signs of fat stranding in the pararenal space and mild swelling of the right kidney suggestive of infection (Fig. 3a). Contrast CT revealed wedge-shaped defects as well as enhancement in the right kidney which suggests that infection has been present for some time (Fig. 3b). She was then diagnosed with AFBN and antibacterial treatment was initiated (Fig. 4). After 3 weeks of antibacterial treatment, chemical analyses and her symptoms improved.
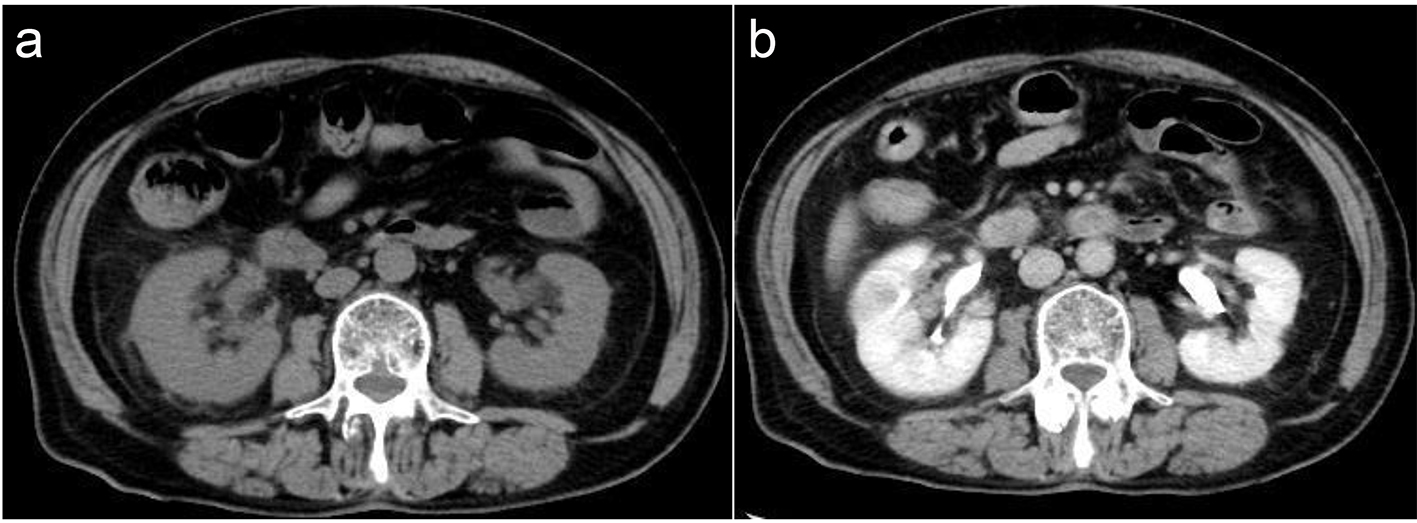 Click for large image | Figure 3. (a) Signs of fat stranding in the pararenal space and mild swelling of the right kidney suggestive of infection. (b) Wedge-shaped detects in the right kidney consistent with AFBN. |
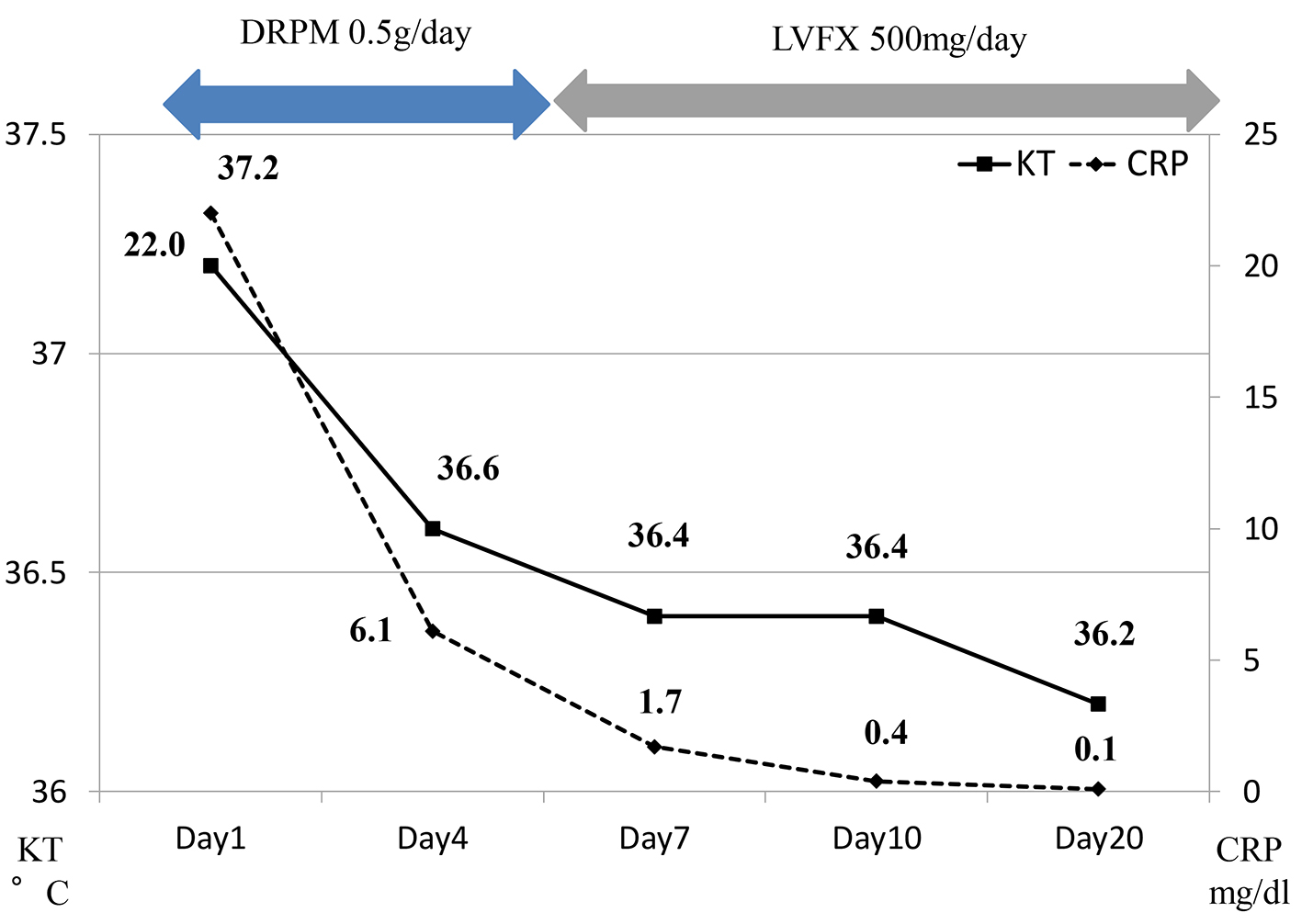 Click for large image | Figure 4. Clinical course of the case 2. DRPM: doripenem; LVFX: levofloxacin. |
| Discussion | ▴Top |
Reports about imaging in patients with acute bacterial renal infection are plagued by inconsistency in terminology; there is no consensus among radiologists, urologists, pathologists, podiatrists, and nephrologists about terms describing acute bacterial infection [1]. Recently, the condition is therefore getting new names, such as AFBN or acute lobar nephronia. AFBN is defined as an acute, localized, and non-liquefactive inflammation of the kidneys caused by bacteria [2]. This strong focal infection may also produce renal abscesses. Clinical symptoms include high fever, shivering, abdominal or back pain, and/or costovertebral angle tenderness. AFBN is common in pediatrics and is considered to be associated with urinary malformation or VUR. Imaging findings for AFBN are characteristic; ultrasonography reveals nephromegaly [3], whereas contrast-enhanced CT reveals oval and wedge-shaped masses with obscure borders and poor contrast enhancement in the arterial phase [4]. However, CT findings sometimes require exclusive diagnosis from liver abscesses and/or malignant renal tumors. As the condition improves, the noticeable shadows seen on CT scans disappear. Recently, there are some reports stressing on role of magnetic resonance imaging (MRI) in diagnosing AFBN, although the modality is expensive and not always available [5, 6].
Underlying conditions that cause AFBN include diabetes mellitus, liver cirrhosis, malignant tumor, ureteral stone, VUR, or neurogenic bladder. The cause of AFBN is bacteremia as well as an ascending infection of Gram-negative bacteria, including E. coli [7]. When antibacterial treatment is initiated before urine culture results are known, the administration of carbapenem or cephem antibiotics is recommended. Even in the acute inflammatory phase of AFBN, there are some cases in which blood and urine cultures are negative for bacteria and urinalyses reveal no hematuria or pyuria. Liping et al [8] reported that, in 14 pediatric cases of AFBN, 28.6% and 71.4% patients revealed negative results for bacteria in urine and blood cultures, respectively. In some cases, AFBN is considered to result from a bloodstream infection. Therefore, AFBN diagnosis is difficult unless contrast-enhanced CT reveals findings indicative of this condition.
In general, AFBN is reported to respond well to antibiotics. However, a few cases of AFBN have reportedly developed septic shock. CT findings for AFBN usually improve in a month after diagnosis and treatment. In some cases, renal resection is required because of recurrence or prolonged infection. Therefore, AFBN should be promptly diagnosed. When patients with an unknown infection present with back pain, headache, or non-generalized fatigue, contrast-enhanced CT should be immediately performed to diagnose or rule out AFBN. A previous study showed that antibiotics administration for 3 weeks was optimal for reducing recurrence [9]. Therefore, long-term administration of antibiotics is recommended as soon as AFBN is diagnosed [10].
In our cases, there were no characteristic symptoms except headache. Tauber et al [11] reported that some AFBN patients present with neurologic symptoms, including consciousness disturbance, nuchal rigidity, and seizure, although their CSF examination was negative. There are reported cases of AFBN patients presenting with headache mimicking meningitis in which CSF examination negated the possibility of meningitis, and CSF culture revealed no pathogens [12, 13]. Fujiwara et al [14] reported the possibility of mild encephalitis/encephalopathy with a reversible splenial lesion accompanying AFBN. These neurologic symptoms are considered to stem from the influence of bacterial cytokines on central nervous system (CNS). High levels of interleukin (IL)-γ and IL-6 are likely related to symptoms of CNS infection. Indeed, Akiba et al [15] reported that the association between AFBN and acute encephalitis/encephalopathy can be explained by increased levels of IL-γ in serum and IL-6 in CSF.
Conclusion
Here, we reported two cases of AFBN without typical symptoms. Bacterial infections accompanied by CNS symptoms are difficult to differentiate from meningitis. Although CSF analyses may be helpful in ruling out meningitis, further investigation to reveal the infection cites should be undertaken. Contrast-enhanced CT scanning is considered to be effective for revealing the origins of infection; therefore, increased use of this modality is recommended in cases of infection with unknown origin.
| References | ▴Top |
- Talner LB, Davidson AJ, Lebowitz RL, Dalla Palma L, Goldman SM. Acute pyelonephritis: can we agree on terminology? Radiology. 1994;192(2):297-305.
doi pubmed - Rosenfield AT, Glickman MG, Taylor KJ, Crade M, Hodson J. Acute focal bacterial nephritis (acute lobar nephronia). Radiology. 1979;132(3):553-561.
doi pubmed - Funston MR, Fisher KS, van Blerk PJ, Bortz JH. Acute focal bacterial nephritis or renal abscess? A sonographic diagnosis. Br J Urol. 1982;54(5):461-466.
doi pubmed - Soulen MC, Fishman EK, Goldman SM, Gatewood OM. Bacterial renal infection: role of CT. Radiology. 1989;171(3):703-707.
doi pubmed - De Pascale A, Piccoli GB, Priola SM, Rognone D, Consiglio V, Garetto I, Rizzo L, et al. Diffusion-weighted magnetic resonance imaging: new perspectives in the diagnostic pathway of non-complicated acute pyelonephritis. Eur Radiol. 2013;23(11):3077-3086.
doi pubmed - Rathod SB, Kumbhar SS, Nanivadekar A, Aman K. Role of diffusion-weighted MRI in acute pyelonephritis: a prospective study. Acta Radiol. 2015;56(2):244-249.
doi pubmed - Cheng CH, Tsau YK, Hsu SY, Lee TL. Effective ultrasonographic predictor for the diagnosis of acute lobar nephronia. Pediatr Infect Dis J. 2004;23(1):11-14.
doi pubmed - Liping J, Zhi C, Ying S, et al. Fourteen (14) cases of acute focal bacterial nephritis in children. Afri J Microbiol Res. 2013;7:3229-3233.
doi - Cheng CH, Tsau YK, Lin TY. Effective duration of antimicrobial therapy for the treatment of acute lobar nephronia. Pediatrics. 2006;117:84-89.
doi pubmed - Boam WD, Miser WF. Acute focal bacterial pyelonephritis. Am Fam Physician. 1995;52(3):919-924.
pubmed - Tauber M, et al. Pediatric Neurology. Principle & Practice. 2006:1571-1594.
- Komatsu H, Yutaka N, Kinoshita D, et al. Report of two elder children with acute focal bacterial nephritis initially suspected of meningitis due to severe extrarenal symptoms. Japanese J Pediatr. 2003;56:1534-1538.
- Yamamoto S, Miura Y, Iseki K. A case of acute focal bacterial nephritis associated with bladder diverticula presenting with meningeal irritation sign. J Clin Pediatr Sapporo. 2005;53:15-18.
- Fujiwara Y, Tanaka F, Wakamiya T, et al. Four cases of mild encephalitis/encephalopathy with a reversible splenial lesion (MERS) accompanying acute focal bacterial nephritis (AFBN). J Jpn Pediatr Soc. 2012;116:1880-1885.
- Akiba T, Ikeda H, Kanai M, et al. A child case of acute focal bacterial nephritis associated with acute encephalitis/encephalopathy. Japanese J Pediatr. 2005;58:839-842.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
