| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website https://www.wjnu.org |
Case Report
Volume 9, Number 2, December 2020, pages 45-51
Management of Ureteric Avulsion During Ureteroscopy: Our Experience in A Case Series
Pulkit Guptaa, Vikram Prabhaa, c, Ritesh Vernekarb, Shisher Devarajua, Sushant Deolea, Priyabrata Adhikara
aDepartment of Urology, JN Medical College, KLE Academy of Higher Education & Research, JNMC Campus, Belagavi-590010, India
bDepartment of Nephrology, JN Medical College, KLE Academy of Higher Education & Research, JNMC Campus, Belagavi-590010, India
cCorresponding Author: Vikram Prabha, Department of Urology, JN Medical College, KLE Academy of Higher Education & Research, JNMC Campus, Belagavi-590010, Karnataka, India
Manuscript submitted September 23, 2020, accepted October 19, 2020, published online November 25, 2020
Short title: Management of Ureteric Avulsion During URS
doi: https://doi.org/10.14740/wjnu417
| Abstract | ▴Top |
Ureterorenoscopy (URS) is usually a safe procedure without any complications. Ureteric avulsion is the most dreaded complication of URS. Most urologists do not have experience in management of ureteric avulsion injuries. Inappropriate management can lead to nephrectomy. Here we are discussing our experience and possible leading factors of this catastrophic complication. We retrospectively reviewed the clinical notes, imaging records, and laboratory investigations of four patients who have been managed for ureteric avulsion in our center during a 12-year period (2008 - 2019). Two cases of lower ureteric avulsion were managed with immediate ureterocystoplasty. Out of which one patient underwent nephroureterectomy. Two cases with total ureteric avulsion were managed with delayed ileal replacement and psoas hitch with Boari flap reconstruction, respectively. During minimum follow-up period of 1 year, no evidence of deterioration in renal function was noted. Use of small caliber scope, proper handling of instruments and minimum forceful manipulation can prevent ureteric avulsion. In experienced hands it can be managed without the requirement of nephrectomy.
Keywords: Ureteric avulsion; Ureteroscopic intracorporeal lithotripsy; Endourology; Complications
| Introduction | ▴Top |
In present era, ureteric calculi are increasingly managed by ureteroscopic intracorporeal lithotripsy. The introduction of the new energy sources and devices, advanced instruments, better optical quality in the last decade has highly improved the success rate of the procedure. Usually it is safe and without complications. The reported rate of complications of ureteroscopy in literature varies from 0.5% to 10% [1-3], which include ureteral false passage, ureteral perforation, bleeding, intussusceptions, and avulsion of the ureter intraoperatively; postoperative complications include infection, fever, urinoma, and stricture formation. The most dreaded of all is ureteric avulsion, which may occur in 0-2% patients [4-6]. With the wide application of ureteroscopes, and endoscopic stone extractors, the incidence of iatrogenic ureteral avulsion tends to grow year by year.
Most of the urologists at present do not have much experience in management of ureteric avulsion injuries. Inappropriate management of this serious condition may lead to nephrectomy [1]. How to manage ureteral avulsion has become a challenge to urologists. Here, we reviewed the management of four cases of ureteral avulsion. In this study, we aimed to discuss our experience and possible leading factors of this serious complication in the light of the current literature.
| Case Reports | ▴Top |
We are presenting our experience with four patients managed for ureteric avulsion at our center (Table 1).
 Click to view | Table 1. Patients Characteristics, Management and Follow-up Details |
Case 1
A 48-years-old female patient with controlled diabetes was operated for 11-mm left lower ureteric stone with moderate hydronephrosis. Patient had previous history of ureterorenoscopy (URS) on ipsilateral side 2 years ago. On URS with 8/9.8Fr semirigid scope, impacted stone was visualized with negotiable narrowing distal to stone about 5 - 6 cm proximal to vesicoureteric junction. Safety guide wire could not be placed. Stone was fragmented with pneumatic lithotripter. Stone grasping forceps was used to remove the fragments which grasped the ureteric mucosa along with it, and lower ureter was inverted in to the bladder while withdrawing forceps. Patient attenders were explained and counseled about the requirement of open exploration. Abdomen was opened through modified Gibson incision. Ragged ureteric edges were freshened and implanted in to anterolateral wall of bladder with Lich-Gregoir technique using 4-0 polyglycolic sutures. The 6Fr 26 cm double J (DJ) stent was placed.
Postoperative follow-up
Pelvic drain was removed on postoperative day (POD) 3 when output was less than 20 mL. Self retaining catheter (SRC) was removed after 1 week. Patient was discharged on the eighth POD. DJ stent was removed after 6 weeks. Patient is on regular yearly follow-up with ultrasound screening which showed maintained adequate parenchymal thickness with no hydronephrosis.
Case 2
A diabetic female patient of 55 years old was operated for mid ureteric 6-mm stone on right side. Patient had history of multiple sittings of extra corporeal shock wave lithotripsy on both sides in the last 5 years. After stone clearance operating surgeon was unable to reach upper ureter as there was severe gripping on 8/9.8Fr semirigid scope. On withdrawing scope was stuck and was not coming out. Feeling of give way was experienced on applying force. Scope was not further withdrawn and patient was planned for immediate open exploration after taking consent. Ureteroscope was removed with difficulty as ureter was tightly gripped over it. Viability of distal ureteric segment was doubtful hence ureterocystoplasty was done in similar way as in case 1.
Postoperative follow-up
Patient did not follow-up after stent removal after 6 weeks until she had fever with loin pain after 8 years. Plain computed tomography of kidney, ureter and bladder (CT KUB) region showed pyonephrosis with gross dilatation and thinned out parenchyma. Ultrasound-guided percutaneous nephrostomy (PCN) was placed and 450 mL frank pus was drained. This relieved the patient but there was no PCN output after the fifth day. Hence laparoscopic nephroureterectomy was done.
Case 3
A female patient aged 53 years old was referred to our emergency room (ER) with complains of fever, pain abdomen and decreased urine output. She had history of left ureteroscopy 3 days back for upper ureteric calculi with total ureteric avulsion. Her serum creatinine on admission was 6.1 mg/dL. Plain CT KUB scan was done, which showed left perinephric urinoma (120 mL) with mild hydronephrosis and ureteric discontinuity at about 2.8 cm from pelviureteric junction (PUJ) and right small kidney (7.4 × 3.4 × 2.9 cm) (Fig. 1). Patient was initially managed with left PCN and perinephric drain placement under ultrasound guidance, which improved her general condition and her creatinine improved to 1.6 mg/dL over 1 week. Her daily PCN output was 1 L. Percutaneous drain (PCD) was removed after 2 weeks. Nephrostogram was done which delineated the pelvis with abrupt cut off.
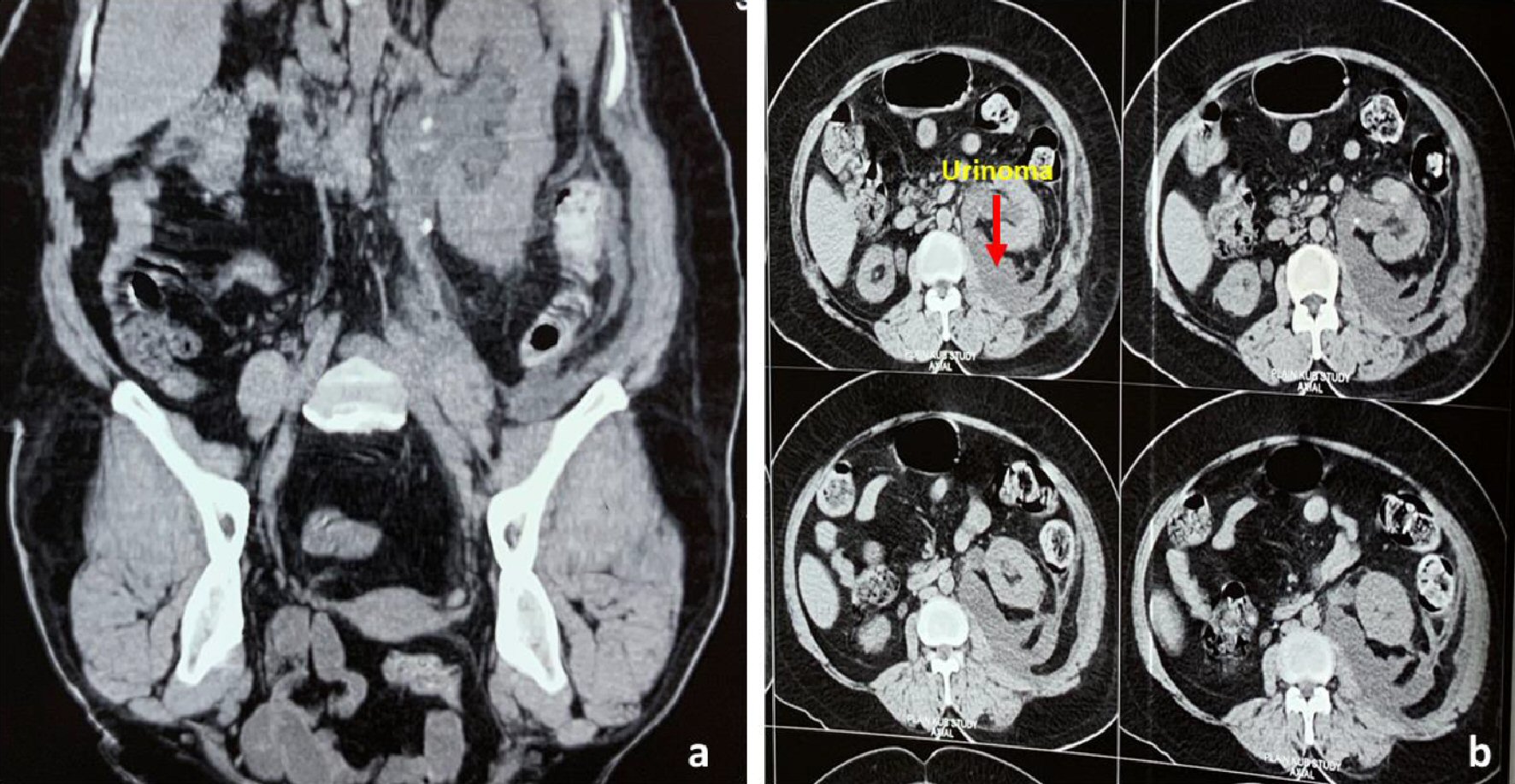 Click for large image | Figure 1. (a) Plain CT KUB (coronal view) showing left upper ureteric injury and residual stone fragments in left pelvicalyceal system. (b) Axial view showing left perinephric urinoma. CT KUB: computed tomography of kidney, ureter and bladder. |
After 6 weeks she was planned for definite management with left uretero-ileal interposition. Preoperative bowel preparation was done. Cystoscopy showed completely obliterated left ureteric orifice and adequate bladder capacity.
Abdomen was opened through midline incision and left colon was retracted medially. Renal pelvis identified and was delineated. About 1 - 2 cm opening was made in renal pelvis. Distal ileal segment (15 cm) with intact mesentery was separated. Upper end of ileal segment was taken through trans-mesocolon in to retroperitoneum and was anastomosed to renal pelvis with interrupted 4-0 polyglycolic sutures, and lower end was anastomosed to full thickness anterior bladder wall in similar fashion (Fig. 2). DJ stent was placed across the anastomosis. Separate suprapubic Malecot catheter was placed in bladder. Also, peri renal and pelvic drain was placed.
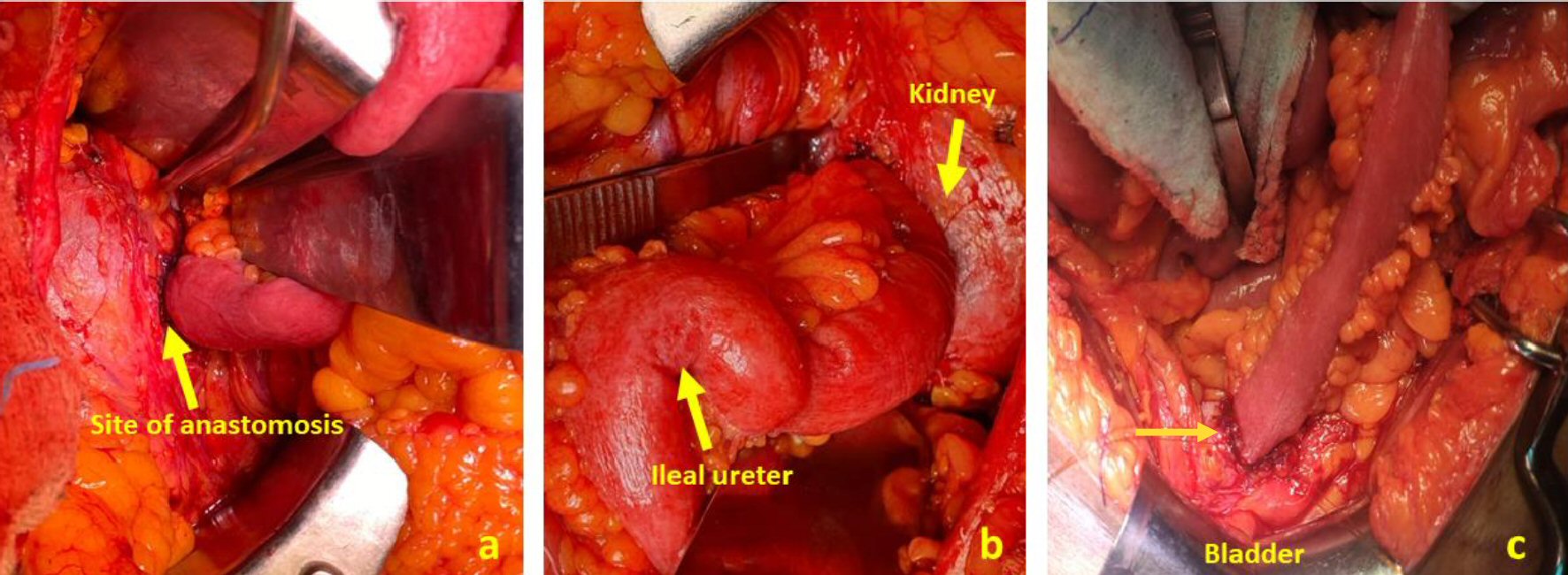 Click for large image | Figure 2. (a, b) Proximal site of anastomosis between renal pelvis and ileum. (c) Ileum anastomosed to anterior bladder wall. |
Postoperative follow-up
Postoperatively patient had hyperkalemia and hypernatremia and acidosis, which were managed accordingly with nephrologist. Perinephric drain was removed after 1 week when output was less than 50 mL. Soda bicarb bladder washes were given for ileal mucus discharge. Patient was discharged after 1 week with suprapubic catheter (SPC) for bladder wash with soda bicarb. SPC was removed after 2 weeks.
Patient is on follow-up since 18 months with three monthly serum creatinine measurements and ultrasonography to detect increasing hydronephrosis. During follow-up period she did not develop any complications and maintained serum creatinine levels at 1.2 mg/dL. There was mild hydronephrosis which did not increase on serial ultrasonography.
Case 4
A 60-year-old male with diabetes and hypertension, total right ureteric avulsion occurred at our institute during semirigid ureteroscopy with 8/9.8Fr ureteroscope for 8-mm upper to mid ureteric calculus with mild hydronephrosis. Impacted stone with edematous ureteric mucosa was visualized in upper mid ureter. Stone was fragmented using pneumatic lithotripter and larger fragments were removed using grasping forceps. There was difficulty in negotiating scope in upper ureter which was gently forced to enter the pelvis. Stiff guide wire was placed. While withdrawing the scope ureter came out over ureteroscope with guide wire in pelvicalyceal system (Fig. 3a). Patient attenders were immediately informed and counseled about unfortunate mishappening and further course of management. Ureteric catheter was passed over guide wire and retrograde pyelography (RGP) was done. Immediate PCN was placed under fluoroscopic guidance. PCN output was about 1 L/day. Patient was discharged with PCN in situ.
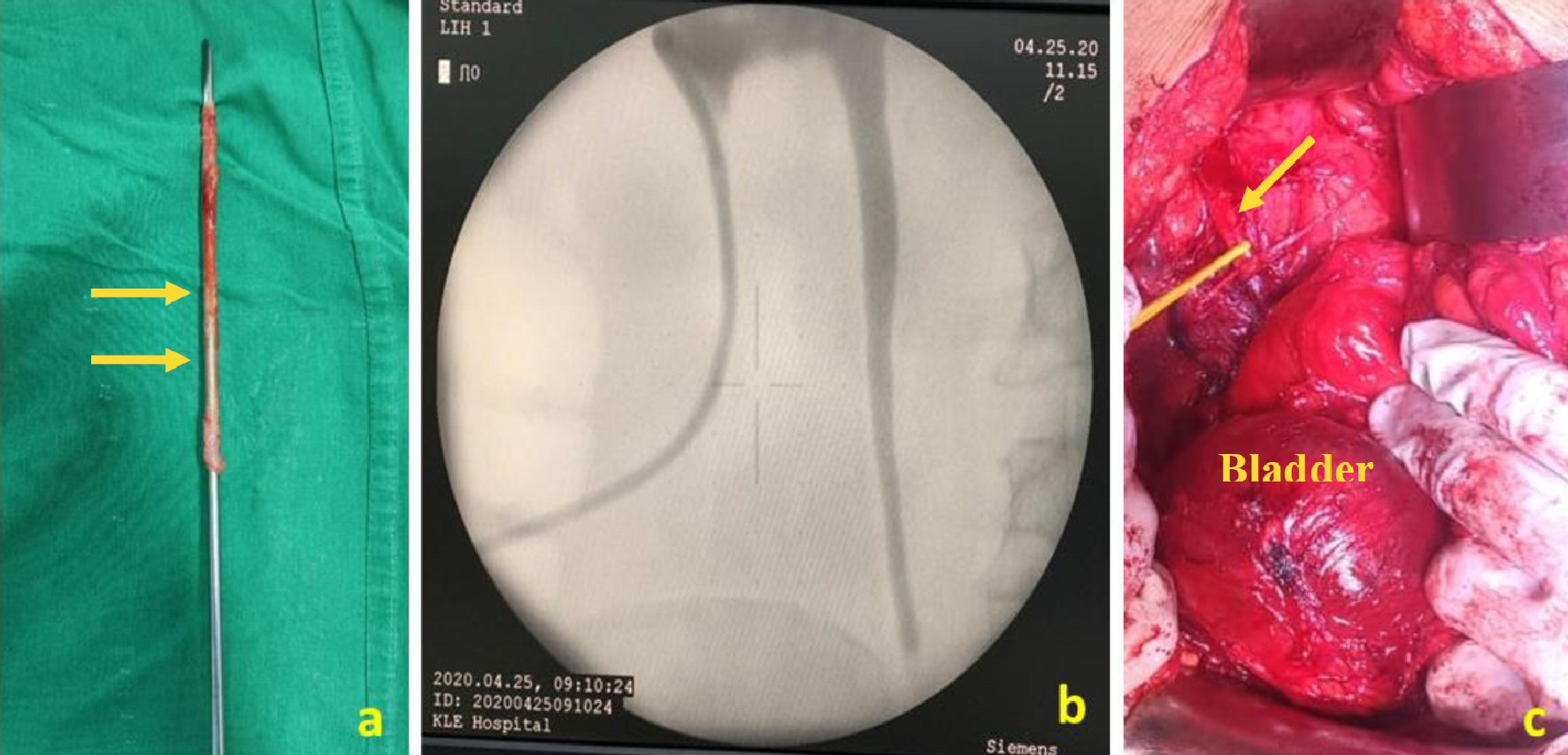 Click for large image | Figure 3. (a) Avulsed ureter tightly gripped over 8/9.8Fr ureteroscope. (b) Nephrostogram showing proximal intact ureter. (c) Looped proximal intact ureter and distended bladder after ligating contralateral superior vesical pedicle. |
On nephrostogram after 6 weeks, 5 - 6 cm of intact ureter was seen and hence, patient was planned for Boari flap reconstruction (Fig. 3b). Abdomen was opened through midline incision. Peritoneum sweeped up and retroperitoneum entered. Ureteric segment was identified and dissected, distal cord like segment incised. Bladder was mobilized well after division of contralateral superior vesical pedicle (Fig. 3c). Defect length was measured to be around 12 cm. Bladder was pulled up and psoas hitch was done to give extra 2 - 3 cm in length. Anterior bladder wall flap based on superior vesicle pedicle of about 12 cm (length) and 5 cm (width) was taken to reconstruct the ureter and end to side full thickness anastomosis of ureter with side of flap fashioned (Fig. 4). DJ stent was placed across the anastomosis. Drain in right paracolic gutter was placed.
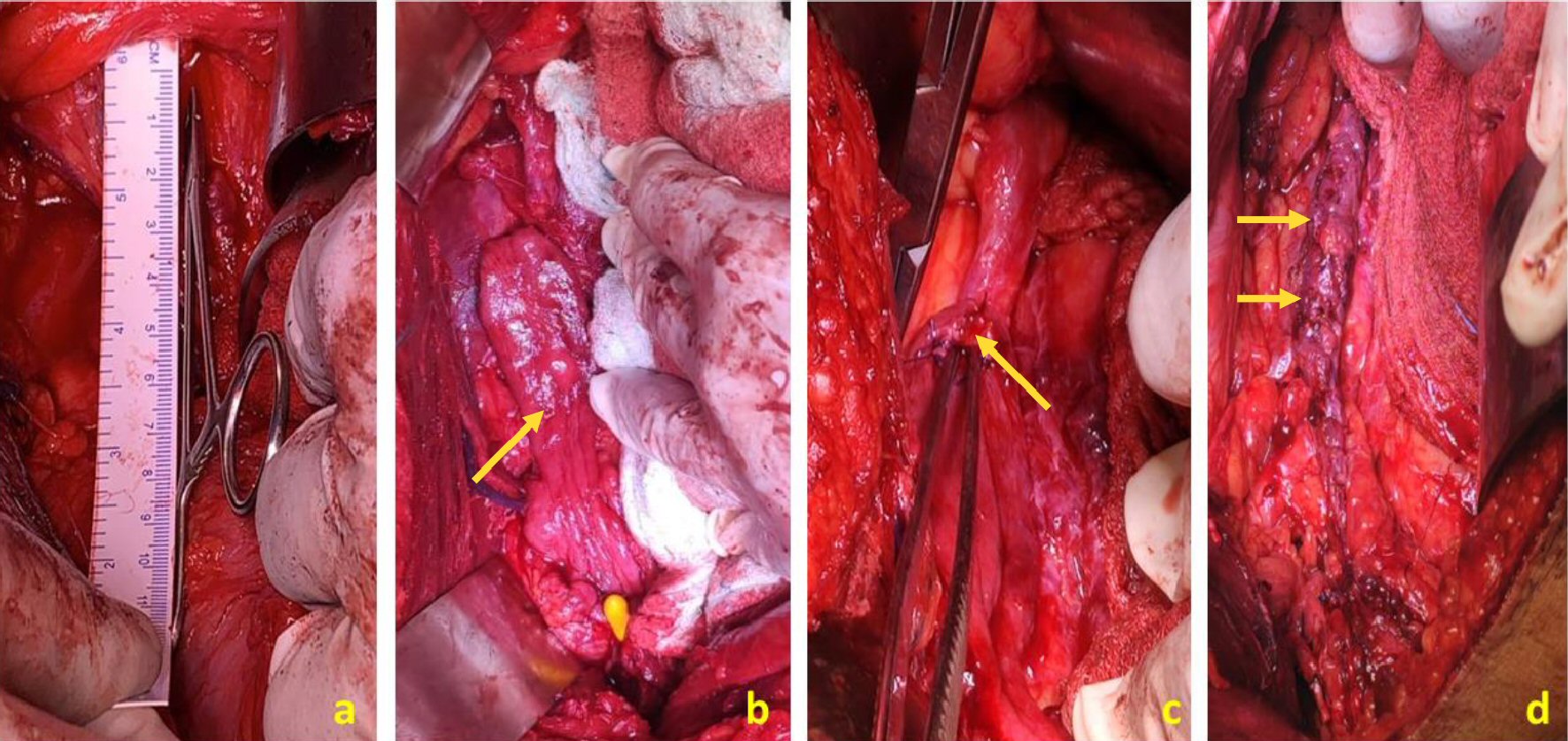 Click for large image | Figure 4. (a) Defect length of about 12 cm measured intraoperatively between ureter and the bladder. (b) Anterior bladder wall flap raised to reconstruct the ureter. (c) Proximal ureter anastomosed to the side of bladder wall flap. (d) Boari flap reconstruction of ureter. |
Postoperative follow-up
Postoperatively drain output was minimal and was removed on POD 3. SRC was removed after 2 weeks. Patient had urgency and frequency after SRC removal which was managed with beta agonists. DJ stent removal was done on out patient basis under local anesthetic after 6 weeks. At 12 months’ follow-up patient had minimal lower urinary tract symptoms with normal creatinine and minimal hydronephrosis with good renal parenchymal thickness.
| Discussion | ▴Top |
Ureteroscopy may lead to various complications; such as stone residuals, mucosal injury, bleeding, perforation, etc., intraoperatively [7]. Other complications such as infection, fever, urinoma, and stricture can be seen in postoperative period. Ureteral avulsion is a rare but serious complication; fortunately, its incidence is only 0-2% as reported in literature [4-6]. Ours being a training institute, minor complications during ureteroscopy such as residual stones, bleeding and minor abrasions are not rare.
Although ureteral avulsion is rare, this catastrophic complication should be taken into consideration while performing ureteroscopy; and urologist should be familiar with management options in different avulsion scenarios. There are not many articles in literature on this complication and its management strategies. Urologists may land up in trouble when they plan a repair procedure due to this unexpected rare serious complication [8]. Patient comorbidities, the age of the patient, the condition of the ipsilateral and contralateral kidney, location and severity of the ureteral damage, patient expectations, and surgeon experience should be taken in to consideration.
Various surgeries have been listed in literature for the reconstruction of ureter depending upon the site and extent of trauma. For distal ureteric injury ureteroneocystostomy with or without posts hitch [9], for mid ureteric injuries Boari flap reconstruction, trans-uretero-ureterostomy are the options. For proximal ureteric injuries uretero-ureterostomy, ureterocalicostomy [10, 11] and other tailored options can be used. Auto transplantation [12, 13] and ileal replacement [14, 15], extended spiral bladder flap [16], pyeloureterostomy plus greater omentum investment outside the avulsed ureter and ureterovesical anastomosis are the options for extensive ureteric injuries [17]. Each procedure has its own pros and cons. Nephrectomy is also reported as an option for extensive injuries of the ureter in the literature [18]. Appendix interposition is also reported as a treatment option for extensive injuries in some literature [19-21].
Ordon et al reported three cases that named it as “the scabbard avulsion”. A nephrostomy tube was placed postoperatively, and finally, all patients underwent a nephrectomy [18]. Unsal et al [22] reported four ureteral avulsion cases in their series, and they performed two Boari flap and two ureteral re-implantation procedures. One of the ureteral reimplantation cases was normal during the follow-up period while the other case developed hydronephrosis.
In our series cases 1 and 2 were managed immediately in the same operation theatre with ureterocystoplasty as lower ureteric injury was suspected. The third patient was in acute renal failure due to obstructive calculus in solitary functioning kidney with total ureteric avulsion at PUJ. So, we decided to perform ileal ureter interposition after stabilizing the patient. In case 4 proximal ureter was intact hence decision to perform Boari flap reconstruction with psoas hitch was taken. We delayed the definitive management for 6 weeks after placing PCN as preoperative consent for repair in case of injury was not taken; moreover it is difficult for patient attenders to accept major surgery when they opted for minimally invasive treatment. Also, delaying the major surgery gives time to improve the nutritional status of the patient if required and for inflammation to settle. So we decided to plan the surgery electively after properly counseling the patient. We realized that it is very important to explain the patient preoperatively the rare possibility of ureteric avulsion and take proper informed written consent. In case of complications attenders and patient should be thoroughly counseled about the injury, further course of management and follow-up, it builds faith in good intention treatment.
Various risk factors for ureteric avulsion are mentioned in the literature which includes chronic stones persisting for more than 3 months, stones larger than 5 mm, dilated proximal ureteral and impacted stones. The muscle in the proximal ureteral tissue is weaker, and therefore, the use of a stone basket to remove the impacted stone in the upper third of the ureter increases the risk of avulsion [8]. A rigid ureteroscopy is also a risk factor for ureteral avulsion as presented in the literature [23, 24].
In our cases avulsion may have occurred due to weak ureteric wall at site of impacted stone with mucosal edema. Use of semirigid 8/9.8Fr ureteroscope, multiple uses of forceps to remove stone fragments and improper handling of instruments by trainee residents may have further contributed.
Ultrasound-guided PCN placement or fluoroscopic PCN placement as in case 3 and 4 helps in tiding over the crisis. Taking the patient immediately for surgery can be appropriate in lower ureteric avulsions. Discussion with experienced urologists and nephrologists involvement when required should be sought. To prevent the ureteric avulsion Ordon et al [18] has suggested the use of a small caliber or flexible ureteroscope, application of lubricant jelly freely along the entire length of the scope or abandon the procedure to repeat on a later occasion after placement of a ureteral stent to allow ureteral dilation if there is strong sense of gripping.
We suggest that 8/9.8Fr ureteroscope should not be used in non-dilated ureters. Safety guide wire can be removed and passed through scope in case of gripping. Also endoscopy is an art of minimum force; unnecessary haste to clear all stone fragments is worthless. It is never sufficient to emphasize that ureteroscope should not be forcefully manipulated and use of safety guidewire and a small-caliber flexible endoscope can save in difficult times.
Conclusions
URS is a very commonly performed minimally invasive treatment for ureteric calculus. Ureteric avulsion is a rare but dangerous complication of URS. Use of small caliber scope, proper handling of instruments and minimum forceful manipulation can prevent ureteric avulsion. The 8/9.8Fr ureteroscope should not be used in non-dilated ureters. Lower ureteric avulsion can be managed immediately while it is better to delay definitive surgery in patients requiring extensive surgery for total ureteric avulsion. Temporary diversion in form of PCN helps in buying time. In experienced hands it can be managed without the requirement of nephrectomy.
Acknowledgments
The authors thank the patients for willing participation in the study.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Patient consent was obtained.
Author Contributions
PG conceptualized and conducted the study, and wrote the manuscript. VP supervised the study and reviewed the manuscript. RV collected the data and reviewed the manuscript. Shishir Devaraju (SD) experimented and reviewed the manuscript. Sushant Deole (SD): data curation. PA: data curation. All the authors read the manuscript, edited and approved the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Al-Awadi K, Kehinde EO, Al-Hunayan A, Al-Khayat A. Iatrogenic ureteric injuries: incidence, aetiological factors and the effect of early management on subsequent outcome. Int Urol Nephrol. 2005;37(2):235-241.
doi pubmed - Butler MR, Power RE, Thornhill JA, Ahmad I, McLornan I, McDermott T, Grainger R. An audit of 2273 ureteroscopies—a focus on intra-operative complications to justify proactive management of ureteric calculi. Surgeon. 2004;2(1):42-46.
doi - Fuganti PE, Pires S, Branco R, Porto J. Predictive factors for intraoperative complications in semirigid ureteroscopy: analysis of 1235 ballistic ureterolithotripsies. Urology. 2008;72(4):770-774.
doi pubmed - Krambeck AE, Murat FJ, Gettman MT, Chow GK, Patterson DE, Segura JW. The evolution of ureteroscopy: a modern single-institution series. Mayo Clin Proc. 2006;81(4):468-473.
doi pubmed - Stoller ML, Wolf JS Jr. Endoscopic ureteral injuries. In: McAninch JW, ed. Traumatic and Reconstructive Urology. 1st ed. Philadelphia: WB Saunders; 1996, p. 199-211.
- Grasso M. Complications of ureteropyeloscopy. In: Taneja SS, Smith RB, Ehrlich RM, eds. Complications of Urologic Surgery 3rd ed. Philadelphia: WB Saunders; 2001, p. 268-276.
- Abdelrahim AF, Abdelmaguid A, Abuzeid H, Amin M, Mousa el S, Abdelrahim F. Rigid ureteroscopy for ureteral stones: factors associated with intraoperative adverse events. J Endourol. 2008;22(2):277-280.
doi pubmed - de la Rosette JJ, Skrekas T, Segura JW. Handling and prevention of complications in stone basketing. Eur Urol. 2006;50(5):991-998; discussion 998-999.
doi pubmed - Gupta V, Sadasukhi TC, Sharma KK, Yadav RG, Mathur R, Tomar V, Yadav SS, et al. Complete ureteral avulsion. ScientificWorldJournal. 2005;5:125-127.
doi pubmed - Ge C, Li Q, Wang L, Jin F, Li Y, Wan J, Lan W, et al. Management of complete ureteral avulsion and literature review: a report on four cases. J Endourol. 2011;25(2):323-326.
doi pubmed - Ben Slama MR, Zaafrani R, Ben Mouelli S, Derouich A, Chebil M, Ayed M. [Ureterocalicostomy: last resort in the treatment of certain forms of ureteropelvic junction stenosis. Report of 5 cases]. Prog Urol. 2005;15(4):646-649.
- Lutter I, Molcan T, Pechan J, Daniel J, Wagenhoffer R, Weibl P. Renal autotransplantation in irreversible ureteral injury. Bratisl Lek Listy. 2002;103(11):437-439.
- Trinchieri A, Montanari E, Salvini P, Berardinelli L, Pisani E. Renal autotransplantation for complete ureteral avulsion following lumbar disk surgery. J Urol. 2001;165(4):1210-1211.
doi - Tanagho EA. A case against incorporation of bowel segments into the closed urinary system. J Urol. 1975;113(6):796-802.
doi - Bazeed MA, El-Rakhawy M, Ashamallah A, El-Kappany H, El-Hammady S. Ileal replacement of the bilharzial ureter: is it worthwhile? J Urol. 1983;130(2):245-248.
doi - Chang SS, Koch MO. The use of an extended spiral bladder flap for treatment of upper ureteral loss. J Urol. 1996;156(6):1981-1983.
doi - Gao P, Zhu J, Zhou Y, Shan Y. Full-length ureteral avulsion caused by ureteroscopy: report of one case cured by pyeloureterostomy, greater omentum investment, and ureterovesical anastomosis. Urolithiasis. 2013;41(2):183-186.
doi pubmed - Ordon M, Schuler TD, Honey RJ. Ureteral avulsion during contemporary ureteroscopic stone management: "the scabbard avulsion". J Endourol. 2011;25(8):1259-1262.
doi pubmed - Lloyd SN, Kennedy C. Autotransplantation of the vermiform appendix following ureteroscopic damage to the right ureter. Br J Urol. 1989;63(2):216-217.
doi pubmed - Juma S, Nickel JC. Appendix interposition of the ureter. J Urol. 1990;144(1):130-131.
doi - Dagash H, Sen S, Chacko J, Karl S, Ghosh D, Parag P, Mackinnon AE. The appendix as ureteral substitute: a report of 10 cases. J Pediatr Urol. 2008;4(1):14-19.
doi pubmed - Unsal A, Oguz U, Tuncel A, Bozkurt OF, Aslan Y, Eraslan A, Senocak C, et al. How to manage total avulsion of the ureter from both ends: our experience and literature review. Int Urol Nephrol. 2013;45(6):1553-1560.
doi pubmed - Martin X, Ndoye A, Konan PG, Feitosa Tajra LC, Gelet A, Dawahra M, Dubernard JM. [Hazards of lumbar ureteroscopy: apropos of 4 cases of avulsion of the ureter]. Prog Urol. 1998;8(3):358-362.
- Alapont JM, Broseta E, Oliver F, et al. Ureteral avulsion as a complication of ureteroscopy. Int Braz J Urol. 2003;29(1):18-23.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
