| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website https://www.wjnu.org |
Case Report
Volume 12, Number 1, July 2023, pages 11-16
A Rare Case of Testicular Plasmacytoma as First Presentation in a Monorchid Patient Without Previous History of Multiple Myeloma: Diagnosis, Management and Review of Literature
Carmelo Agostino Di Francoa, f, Sandro Bellaviab, Carmela Emmanueleb, Genziana Buttafuocob, Francesco Faillaa, Enrico Grimaldia, Leonardo Lizzioa, Emilio Malacasaa, Tommaso Torrea, Giuseppe Restivoc, Francesca Maria Di Francod, Lavinia Galvagnoe, Giovanni Bolognaa
aUrology Department, Umberto I Hospital, Enna, Italy
bPathology Department, Umberto I Hospital, Enna, Italy
cNephrology Department, Umberto I Hospital, Enna, Italy
dPsychology and Psychotherapy Service, Enna, Italy
eLanguage and Translation Services, Enna, Italy
fCorresponding Author: Carmelo Agostino Di Franco, Urology Department, Umberto I Hospital, Enna, Italy
Manuscript submitted April 25, 2023, accepted June 5, 2023, published online July 24, 2023
Short title: Testicular Plasmacytoma in a Monorchid Patient
doi: https://doi.org/10.14740/wjnu441
| Abstract | ▴Top |
Testicular plasmacytoma is a rare disease with few described cases in literature since 1939 when the first case was described. Testicular plasmacytoma can occur as first presentation disease or in multiple myeloma relapse. We report a case of a monorchid asymptomatic 70-year-old patient without previous multiple myeloma diagnosis with incidental discovery of right testicular mass who presented with rapid worsening of myeloma-related symptoms immediately after orchifunicolectomy. Diagnosis was made in our urology department and patient was referred to hematologist for continued therapy. We will discuss the case and review the literature.
Keywords: Testis cancer; Testicular plasmacytoma; Testis myeloma; Metastasis; Testis metastasis
| Introduction | ▴Top |
Multiple myeloma is a neoplastic disorder characterized by malignant proliferation of plasma cells within the body’s bone marrow. Multiple myeloma may present with renal function impairment, hypercalcemia, anemia and osteolytic bone lesions.
Most patients with a plasma cell neoplasia show diffuse marrow involvement at presentation, but extramedullary forms (extramedullary plasmacytoma (EMP)) and the “leukemic” variety are less common.
EMP has been reported most commonly in the respiratory tract, head and neck region, gastrointestinal tract and central nervous system [1]. Plasmacytomas can be primary lesions or they can be indicators of progressive disease [2, 3].
Testicle is a very rare site for EMP; since the first reported case in 1939, less than 70 cases are described in literature [4]. Among testicular cancers, plasmacytoma is a rare entity, with an overall incidence of 0.03% to 0.1% [5, 6].
In the literature, we found few cases of testicular plasmacytoma in patients without a previous diagnosis of multiple myeloma [7-9]. In fact, the most described cases are in patients with a known multiple myeloma diagnosis or in patients developing disseminated disease later in life [10-12]. In addition, this is the first case described in a monorchid patient.
| Case Report | ▴Top |
We report the case of a 70-year-old man in good general conditions, monorchid due to left cryptorchidism treated with left orchifunicolectomy in pediatric age, who presented to our outpatient clinic during a routine urological check-up. Basic blood tests were all normal except for mild increase of uric acid (7.2 mg/dL). Patient had history of urinary stones in the past. The patient had no previous significant medical history except for well-controlled hypertension with angiotensin-converting enzyme (ACE) inhibitor.
Physical examination and ultrasound were negative for urinary stones but minimal right pelviectasis was identified. During genital examination, right testis appeared slightly increased in volume and hard to touch without evoked pain. Right testis ultrasound showed heterogeneously echoic testicular mass with increased color-Doppler vascular signals; epididymis was normal. Bilateral inguinal ultrasound was negative for enlarged lymph nodes. Testicular markers (lactate dehydrogenase, β-human chorionic gonadotropin and alpha-fetoprotein) were normal. At this point, right orchifunicolectomy and computed tomography (CT) scan to study right renal pelviectasis were indicated.
After 1 week, preoperative blood tests showed hemoglobin of 10.5 g/dL, normal white blood cells and platelets, creatinine of 1.6 mg/dL, normal azotemia, uric acid of 7.2 mg/dL, calcium of 10.6 mg/dL, normal sodium and potassium, and mild proteinuria in morning urinalysis. Preoperative testosterone level was normal. Patient remained asymptomatic except for very mild right lumbar pain. We decided to perform abdominal CT scan without contrast (due to creatinine value): CT scan was negative for ureteral calculi and no retro peritoneal masses or lymph nodes were reported.
After 1 day, right radical orchifunicolectomy with spinal anesthesia was performed with no complications. Antibiotic prophylaxis with ceftriaxone 1 g was administered. Patient received good post-operative hydration and diuresis was normal. On first post-operative day, blood test showed a drastic increase in serum creatinine (4.2 mg/dL), increased serum uric acid (10.2 mg/dL),calcium of 11 mg/dL, normal serum sodium and potassium concentrations with normal urine output. The patient reported worsening of right lumbar/costal pain and a temperature of 38 °C. Procalcitonin was normal during the entire hospitalization. Review of previous CT scan showed a small right XI rib osteolytic lesion. Nephrology evaluation was performed: patient was hydrated and allopurinol therapy was started. Blood tests showed progressive reduction in serum creatinine, uric acid and calcium levels. After 1 week, creatinine value was stable at 3.1 mg/dL, calcium was 10.5 mg/dL, hemoglobin was 10.2 g/dL, with normal white blood cells and platelets counts. Surgical wound was healing well during the entire hospitalization. Serum protein electrophoresis showed a gamma-spike and urine electrophoresis showed monoclonal light chains (Fig. 1). Serum IgA level was high (2,016 mg/dL) with low IgG and IgM levels (430 and 11 mg/dL, respectively). Head CT scan was negative for bone lesions.
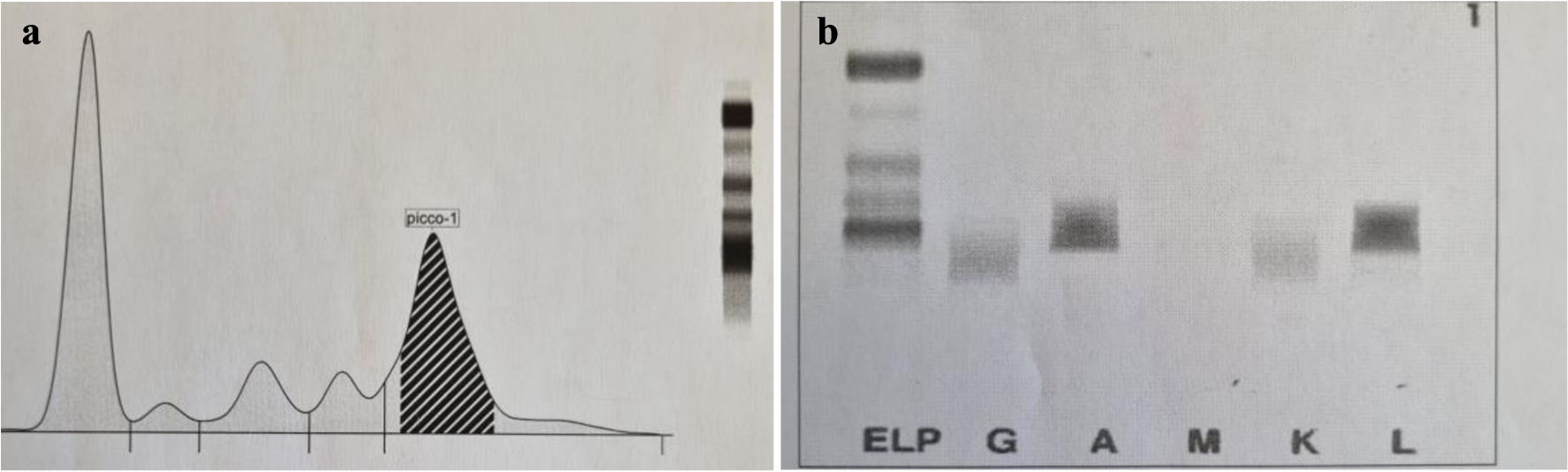 Click for large image | Figure 1. (a) Electrophoresis of serum protein showing gamma-spike. (b) Urine electrophoresis showing monoclonal light chains. |
One week after orchiectomy, we performed a serum testosterone level confirming hypogonadism but testosterone replacement therapy was not started at the moment because of hypercalcemia.
In addition, patient started weekly psychotherapy and hypnotherapy with Ericksonian approach due to mild depressive status with good outcome.
On gross examination, the testis showed increased size (7 × 4.5 × 2.5 cm) and had a solid consistency. At cutting, there was a neoformation sized 3.3 × 2.5 cm, variegated in appearance, soft, fleshy, with necrotic and hemorrhagic areas (Fig. 2). Plasmacytomas of testis can be mistaken for other types of tumors, including seminoma, lymphoma and metastatic melanoma. On microscopic examination, the neoplasm consisted of sheets of plasmacytoid cells of varying degrees of differentiation. A population of more immature cells predominated, with a higher nuclear/cytoplasmic ratio, scattered nuclear chromatin and often prominent nucleoli, and plasmablastic elements characterized by a less abundant cytoplasm with sparse or absent halo region, fine reticular chromatin and large nucleus (Fig. 3). A smaller population of well-differentiated or mature plasma cells was present. These cells are characterized by abundant basophilic cytoplasm, perinuclear halo region, eccentric round nuclei, “clock-like” chromatin, and inconspicuous nucleoli.
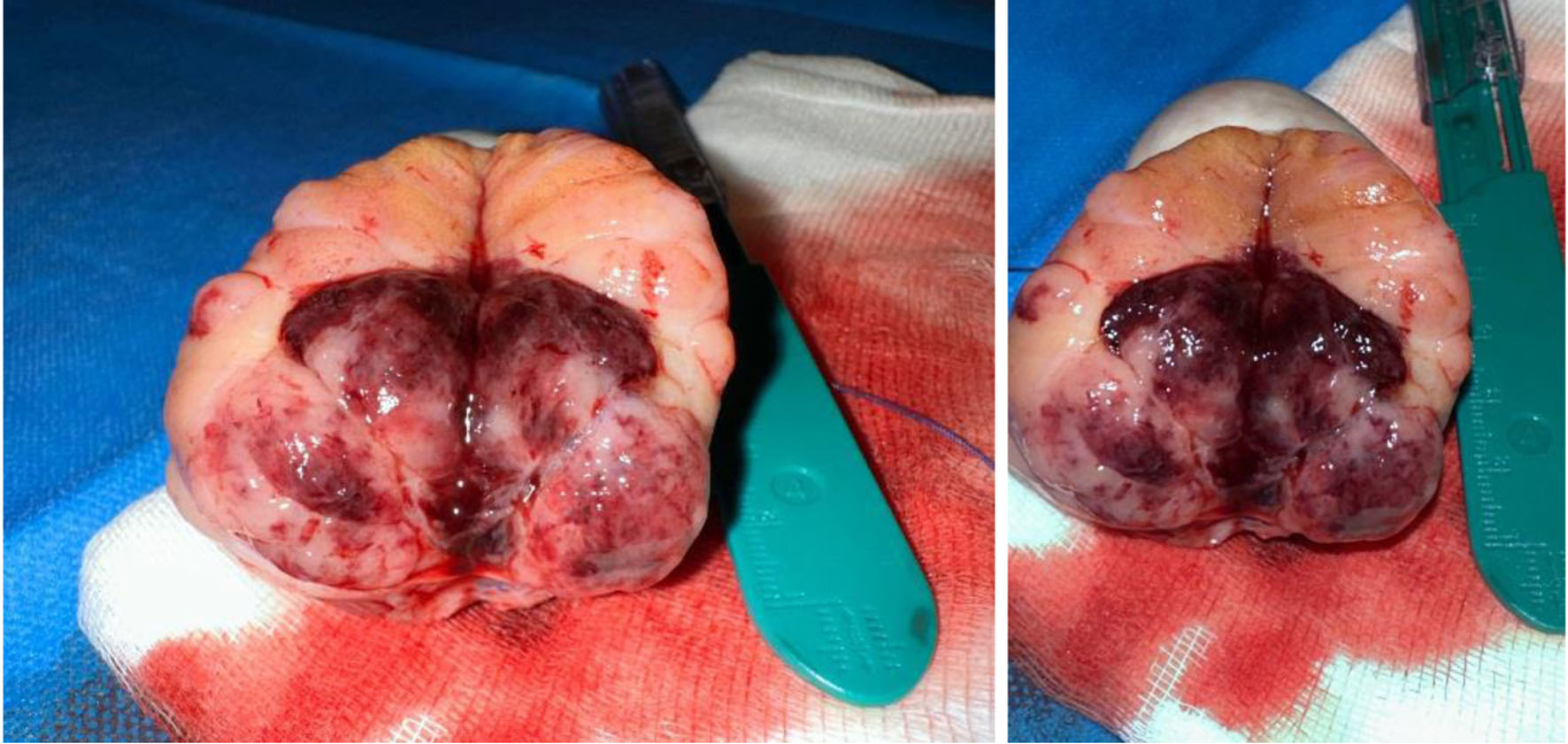 Click for large image | Figure 2. On gross examination, testis showed neoformation sized 3.3 × 2.5 cm, variegated in appearance with necrotic areas. |
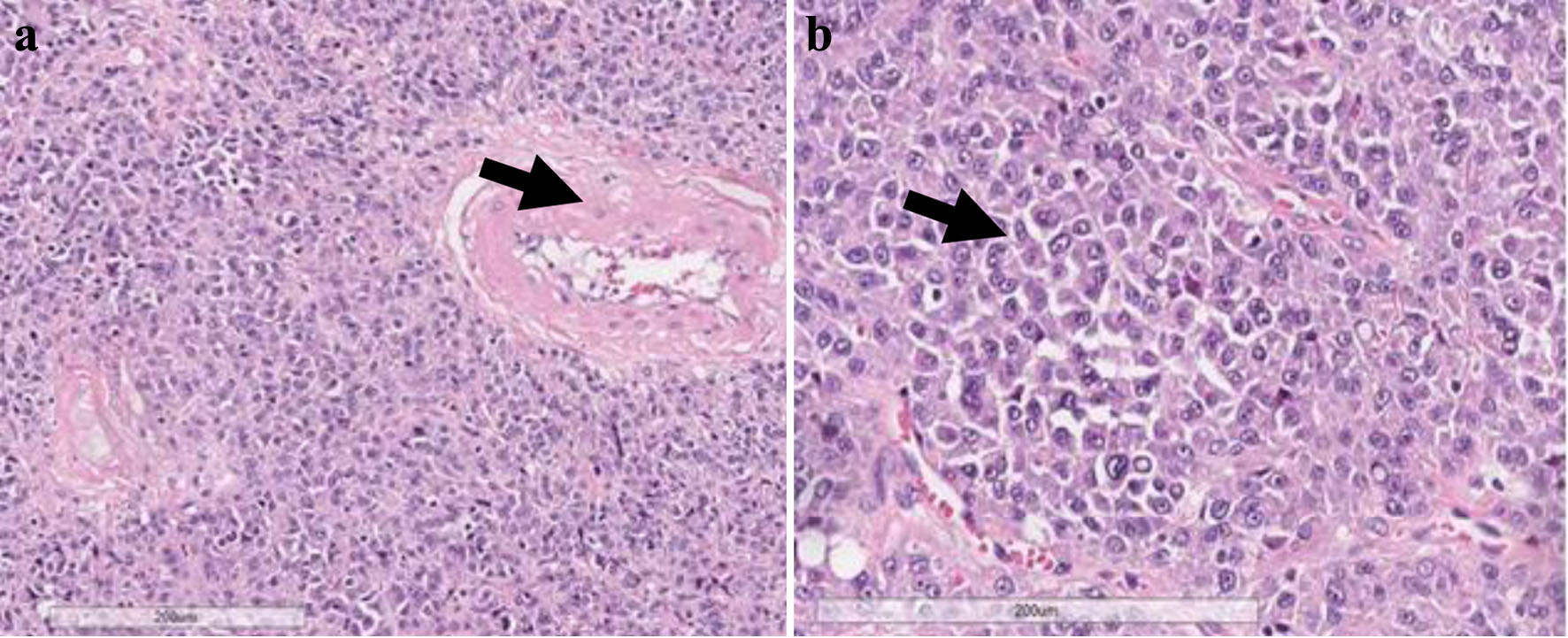 Click for large image | Figure 3. (a) Diffuse infiltration of atypical plasma cells surrounding atrophic seminiferous tubule (arrow) (hematoxylin and eosin; × 200). (b) A population of immature and anaplastic plasma cells predominated, with a higher nuclear/cytoplasmic ratio, scattered nuclear chromatin and often prominent nucleoli, with occasional intracellular small vacuoles (arrow) (hematoxylin and eosin; × 400). |
Perilesional testicular parenchyma showed advanced atrophy, characterized by small tubules with thick basal membranes and few or no germ cells; interstitial tissue showed varying degrees of edema and fibrosis with an increased numbers of Leydig cells. As shown in the figures, neoplastic plasma cells expressed CD38 and CD138 and MUM1, had aberrant expression of CD117 and partial expression of CD45, and were negative for CD20 (Fig. 4).
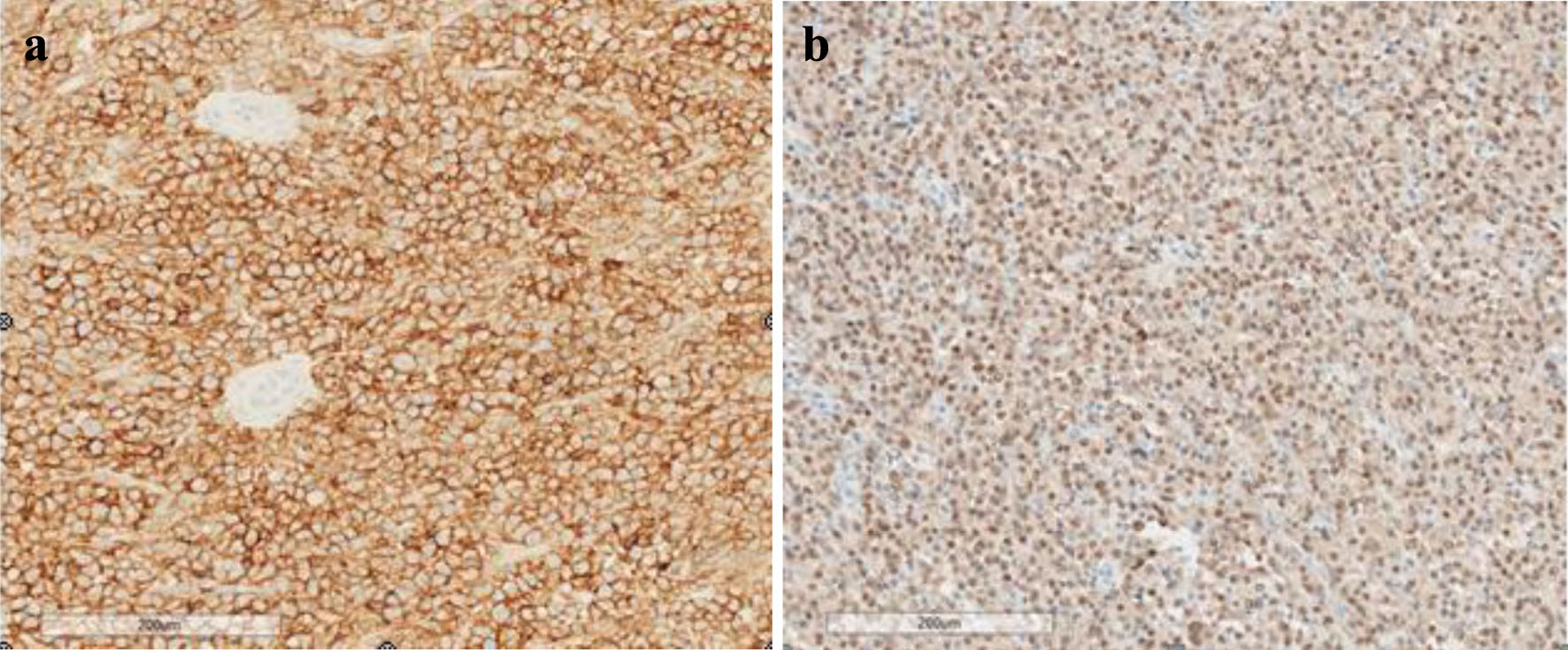 Click for large image | Figure 4. Neoplastic plasma cells showing immunohistochemical expression of CD38 at the membrane level (a) and nuclear staining of MUM1 (b) (× 200). |
Immunohistochemical study with antibodies against kappa and lambda light chains is an important approach for the evaluation of suspected plasmacytoma; a population restricted to kappa or lambda light chains confirms the diagnosis of plasmacytoma (Fig. 5). In this case, restriction to lambda chains was confirmed.
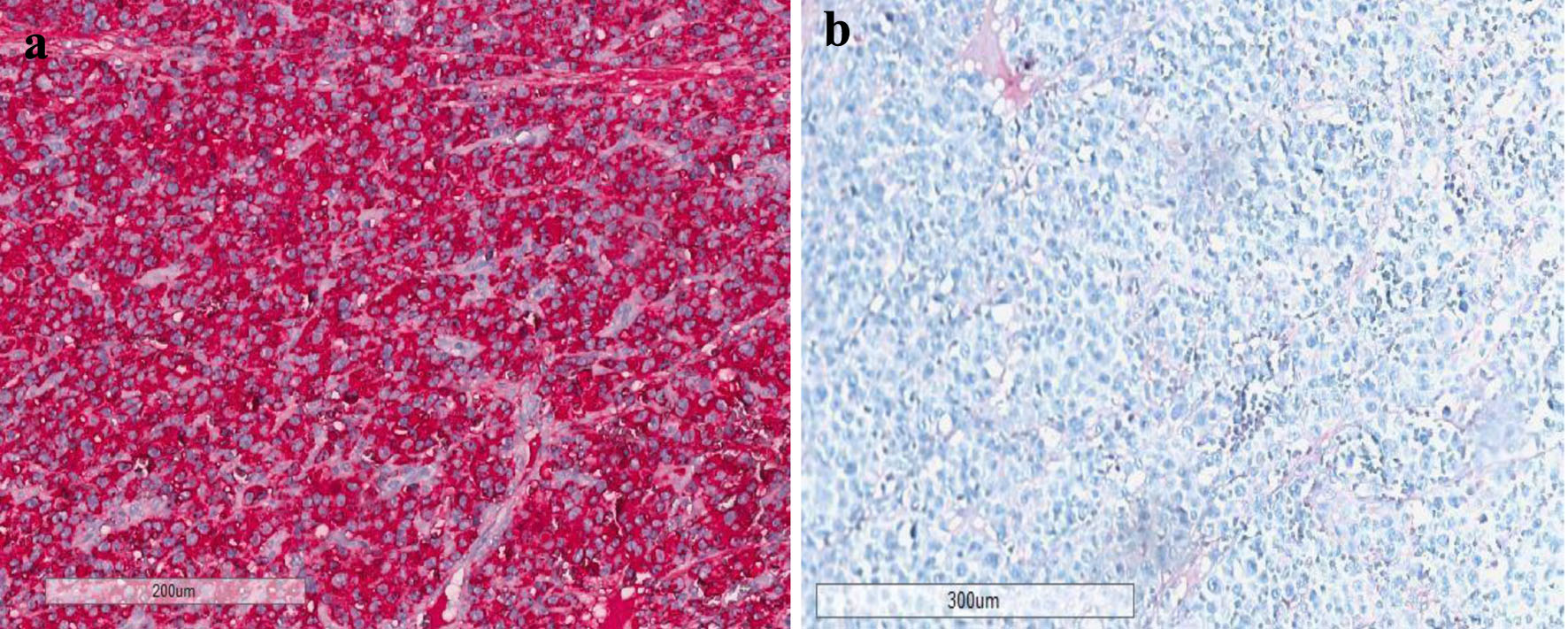 Click for large image | Figure 5. (a) Immunohistochemical study confirming the monoclonality of neoplastic process by showing restriction to lambda light chains (a, × 200) and negativity to kappa chains (b ,× 170). |
| Discussion | ▴Top |
EMP is a rare form of plasma cell neoplasm, and often presents concurrently with multiple myeloma, but can present as an isolated tumor. Patients with isolated plasmacytoma have high rates of progression to multiple myeloma later in life. For this reason, it is important to diagnose plasmacytoma and survey these patients appropriately for progression to disseminated disease.
Plasmacytoma of the testicle is exceedingly rare, but a disease to consider in patients presenting with testicular mass, particularly in elderly patients in which testicular cancer incidence is relatively low. When plasmacytoma occurs in the testis, the diagnosis can be difficult, often resembling other more common causes of testicular mass, and requires multiple diagnostic tests for accurate diagnosis.
Multiple myeloma is a plasma cell tumor that affects bone marrow characterized by synthesis and excretion of monoclonal proteins. In some cases, tumor cells can be located in extramedullary sites. Most frequent extramedullary locations are kidney, nasopharynx and paranasal sinus, lymph nodes, spleen, lung, pancreas, pleura and pericardium, and skeletal muscle [13].
Testicular plasmacytoma incidence is around 0.03% and 0.1% of testicular cancers and represents only 2% of plasma cell neoplasm [14]. In addition, testicular plasmacytoma usually occurs in patients with known systematic multiple myeloma, either at the diagnosis or at relapse [15]. The first described case of testicular plasmacytoma was in 1939 [16].
As reported by Oppenheim et al [17], plasmacytoma of the testis is seldom diagnosed as a primary event. In this study, only six out of 37 cases were solitary plasma cell neoplasias of the testis, while the others developed in patients previously diagnosed with multiple myeloma.
In the literature, extramedullary multiple myeloma is described in 6-8% of patients at the time of diagnosis and 10-30% in relapsed disease [18], whereas testicular localization, in patients known with myeloma is a rare entity around 4% of cases [19]. The median age of presentation for EMP is 55 - 59 years, lower than myeloma multiple [20].
In the literature, testicular plasmacytoma is considered a rare entity with around 70 described cases [21]. Testis is defined as a sanctuary site for hematological cancers because of the presence of testicular blood barrier and this is important during the evaluation of a patient with history of multiple myeloma.
Hayes et al performed autopsies on 38 patients with multiple myeloma with EMP and found evidence of testicular involvement in only one case. They further reviewed the literature going over 182 cases with similar demographics and found only five cases of EMP with testicular involvement [3]. Pasmantier and Azar [2] performed 57 autopsies of patients with EMP and they did not report any cases of testicular involvement.
Plasmacytoma of testis is usually treated by radical orchifunicolectomy and in some cases, when it is in an advanced stage or recurrence is present, radiotherapy can be added. In cases of multiple cancer lesions, chemotherapy or monoclonal antibodies are indicated [22].
Testicular plasmacytoma can be the first manifestation of multiple myeloma or evidence of recurrence of myeloma but most often it shows no clinical manifestations and it is discovered on autopsy [23] in patients with multiple myeloma history.
The prognosis of testicular plasmacytoma depends on co-presence of myeloma. In fact in presence of multiple myeloma, prognosis is poor and most patients show disease progression [13].
In addition, most of patients with a prior diagnosis of testicular plasmacytoma will develop multiple myeloma with only a few long-term progression-free survival cases described [24].
In our case, patient had asymptomatic rib lesion at diagnosis and mild renal failure but we suspected some hematological disease only after orchifunicolectomy due to the rapid worsening of renal function, fever and rib pain on first post-operative day. We think that this rapid worsening of symptoms can be explained by immunostimulation induced by surgical stress; patient received subarachnoid anesthesia, the only parenteral drug given was ceftriaxone. Orchifunicolectomy was performed by clamping sperm cord before any testis manipulation, so we think that malignant cells dissemination is unlikely.
In addition, this case can be a management challenge to choose the correct approach in terms of hypogonadism but we decided not to start any testosterone replacement therapy, in accordance with the hematological team and the patient. Psychotherapy can be useful in these cases to delay the start of testosterone replacement therapy.
Conclusions
Testis plasmacytoma is a rare disease with few cases described in literature. Our case is interesting because testicular mass represents the first presentation of multiple myeloma with rapid progression of symptoms immediately after orchiectomy in a monorchid patient. Medical management requires a multidisciplinary approach and in this specific case timely diagnosis has been fundamental for the patient outcome and for his quality of life.
Acknowledgments
We would like to express our sincere gratitude to all the individuals and organizations that have contributed to the publication of this research paper, in particular the nephrology department equipe of Enna Umberto I Hospital: Dr. C. Cannarozzo, Dr. G. Ferrara, Dr. R. Salemi.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
This case report did not require informed consent.
Author Contributions
Carmelo Agostino Di Franco is the main author, he performed the first diagnosis and clinical management of the patient, collected data and wrote the article. Sandro Bellavia, Genziana Buttafuoco and Carmela Emmanuele performed research in particular pathology analysis; Francesco Failla, Enrico Grimaldi, Leonardo Lizzio, Emilio Malacasa, Tommaso Torre, and Giuseppe Restivo supported the author in data collection; Francesca Maria Di Franco performed the psychology support to the patient. Lavinia Galvagno performed language and translation support. Giovanni Bologna is the Urology Ward Chief and supported the group during diagnosis and surgical treatment.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Kapadia SB. Multiple myeloma: a clinicopathologic study of 62 consecutively autopsied cases. Medicine (Baltimore). 1980;59(5):380-392.
pubmed - Pasmantier MW, Azar HA. Extraskeletal spread in multiple plasma cell myeloma. A review of 57 autopsied cases. Cancer. 1969;23(1):167-174.
doi pubmed - Hayes DW, Bennett WA, Heck FJ. Extramedullary lesions in multiple myeloma; review of literature and pathologic studies. AMA Arch Pathol. 1952;53(3):262-272.
pubmed - Lue K, Emtage JB, Parinas MA, Dhillon J, Pow-Sang J. An extramedullary plasmacytoma in the testicle: A case report and review of the literature. Can Urol Assoc J. 2015;9(3-4):E240-242.
doi pubmed pmc - Chica G, Johnson DE, Ayala AG. Plasmacytoma of testis presenting as primary testicular tumor. Urology. 1978;11(1):90-92.
doi pubmed - Levin HS, Mostofi FK. Symptomatic plasmacytoma of the testis. Cancer. 1970;25(5):1193-1203.
doi pubmed - Hassen-Troudi F, Mege-Lechevallier F, Colombel M, Scoazec JY. [Testicular localisation of a plasmocytoma]. Ann Pathol. 2009;29(1):32-35.
doi pubmed - Anghel G, Petti N, Remotti D, Ruscio C, Blandino F, Majolino I. Testicular plasmacytoma: report of a case and review of the literature. Am J Hematol. 2002;71(2):98-104.
doi pubmed - Walker FB, Bluth EI, Kenney A, Beckman EN. Plasmacytoma of the testis. J Ultrasound Med. 2005;24(12):1721-1725.
doi pubmed - Matsuda Y, Kato R, Miyao N, Sato S, Konishi Y, Kon S. [A case of extramedullary plasmacytoma of testis converted to multiple myeloma]. Hinyokika Kiyo. 2010;56(10):593-595.
pubmed - Hou TY, Dai MS, Kao WY. Testicular plasmacytoma with bone dissemination without medullary plasmacytosis. Ann Hematol. 2003;82(8):518-520.
doi pubmed - Tanagho Y, Stovsky M, Maclennan GT. Testicular plasmacytoma. J Urol. 2010;184(3):1161-1162.
doi pubmed - Khan M, Rajarubendra N, Azer S, Skene A, Harrison SJ, Campbell B, Lawrentschuk N. Plasmacytoma of the testis in a patient with relapsed and refractory multiple myeloma: Case report and review of the literature. Urol Ann. 2015;7(4):530-533.
doi pubmed pmc - Alvarez-Mugica M, Jalon Monzon A, Bulnes Vazquez V, Aguilar Andrea C, Fernandez Gomez JM, Gonzalez Alvarez RC, Regadera Sejas FJ. Secondary testicular plasmocytoma. Arch Esp Urol. 2007;60(1):99-102.
pubmed - Croake A, Hall M, Zhang X, Dogra V. Bilateral testicular plasmacytomas. American Journal of Sonography. 2020;1:4.
doi - Ulrich H. Multiple myeloma. The Archives of Internal Medicine. 1939;64:994.
- Oppenheim PI, Cohen S, Anders KH. Testicular plasmacytoma. A case report with immunohistochemical studies and literature review. Arch Pathol Lab Med. 1991;115(6):629-632.
pubmed - Vusqa UT, Asawa P, Fazal S, Samhouri Y. Testicular plasmacytoma masking as epididymo-orchitis in a known multiple myeloma patient. Cancer Diagn Progn. 2022;2(5):549-552.
doi pubmed pmc - Strauss D, Sachpekidis C, Dapunt U, Goldschmidt H, Dimitrakopoulou-Strauss A. Unusual extramedullary manifestation in multiple myeloma: bilateral synchronous testicular infiltration. Clin Nucl Med. 2023;48(2):e76-e77.
doi pubmed - Galieni P, Cavo M, Pulsoni A, Avvisati G, Bigazzi C, Neri S, Caliceti U, et al. Clinical outcome of extramedullary plasmacytoma. Haematologica. 2000;85(1):47-51.
pubmed - Manolitsis I, Tzelves L, Koutoulidis V, Gavriatopoulou M, Varkarakis I. Metachronous bilateral testicular plasmacytoma after an initial soft tissue, extramedullary plasmacytoma. Cureus. 2021;13(11):e19517.
doi pubmed pmc - Shimokihara K, Kawahara T, Chiba S, Takamoto D, Yao M, Uemura H. Extramedullary plasmacytoma of the testis: A case report. Urol Case Rep. 2018;16:101-103.
doi pubmed pmc - Hathaway AR. Incidental discovery of a testicular plasmacytoma at initial presentation of multiple myeloma. Case Rep Hematol. 2013;2013:752921.
- Filho MG. Primary testicular plasmocytoma: A five year follow-up. Urol Ann. 2013;5(1):39-41.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
