| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website http://www.wjnu.org |
Case Report
Volume 2, Number 1, June 2013, pages 29-32
Primary Clear Cell Adenocarcinoma in a Female Urethral Diverticulum: A Case Report and Review
Guy Sheahana, b, Antonio Vega Vegaa
aUrology Department, Rockhampton Base Hospital, Australia
bCorresponding author: Guy Sheahan, Urology Department, Rockhampton Base Hospital, Queensland Health, Australia
Manuscript accepted for publication May 27, 2013
Short title: Primary Clear Cell Adenocarcinoma
doi: https://doi.org/10.4021/wjnu67w
| Abstract | ▴Top |
Clear Cell Adenocarcinoma is a very rare variant of lower urinary tract malignancy. We present a 54 years old lady who presented with haematuria and a urethral mass on ultrasound. MRI subsequently demonstrated a heterogeneous mass within a urethral diverticulum. Biopsies of the mass demonstrated clear cell adenocarcinoma with clearing of the cytoplasm, moderate nuclear pleomorphism. Immunohistochemically cells were positive for: cytokeratin 7 and p16, p53, CA125, CAM5.2, AE1/AE3. They were negative for: thrombomodulin, oestrogen, progesterone, cytokeratin 20, p63, CD10, CEAP, WT1, AFP, s100. She underwent anterior exenteration with pelvic lymphadenectomy, and ileal conduit formation. Histology of which demonstrated surgically clear margins but 3/6 positive lymph nodes. She underwent 50.4Gy for consolidative radiotherapy given the lack of known benefit for chemotherapy. Subsequent PET scans have demonstrated lymphatic disease progression, but remains alive one year after diagnosis.
Keywords: Clear cell adenocarcinoma; CCA; Urethral diverticulum; Mesonephric tumour; Urothelial carcinoma; Mullerian; Anterior exenteration
| Introduction | ▴Top |
Clear cell adenocarcinoma (CCA) is a very rare variant of cancer the lower urinary tract; with approximately 100 previous case reports since 1968 [1]. Given its rarity, our understanding of this disease remains very limited. This case report provides an opportunity to review the literature and help correlate some of the features most commonly found with clear cell adenocarcinoma.
| Case Report | ▴Top |
A 54 years old post menopausal lady was referred by her family physician/general practitioner (GP) to an urologist for investigation and management of a twelve month history of urinary hesitancy, reduced urine stream calibre and intermittent episodes of hematuria. Further medical history elucidated that she was a current smoker ten per day, has four children and had regular normal cervical smears. Surgical history included a laparotomy for an ectopic pregnancy and associated endometriosis. Vaginal examination revealed a 3.5 cm non tender, tense, minimally mobile sub-urethral cystic lesion. Urine culture was unremarkable as were her baseline bloods. Ultrasound arranged by her GP demonstrated a heterogenous hypoechoic cystic type mass around her urethra.
Magnetic resonance imaging (MRI) demonstrated a 3.7× 4.1 cm mass with solid and cystic areas wrapping around the urethra (Fig. 1). The prominent polypoidal solid areas in the anterior component of the mass were suggestive of a transitional cell malignancy. Urine cytology showed malignant cells consistent with urothelial carcinoma. Based on the images and cytology results the patient underwent urgent cystourethroscopy, this demonstrated a mass in the posterior wall diverticulum of the urethra. Multiple biopsies were obtained via a transurethral and transvaginal approach.
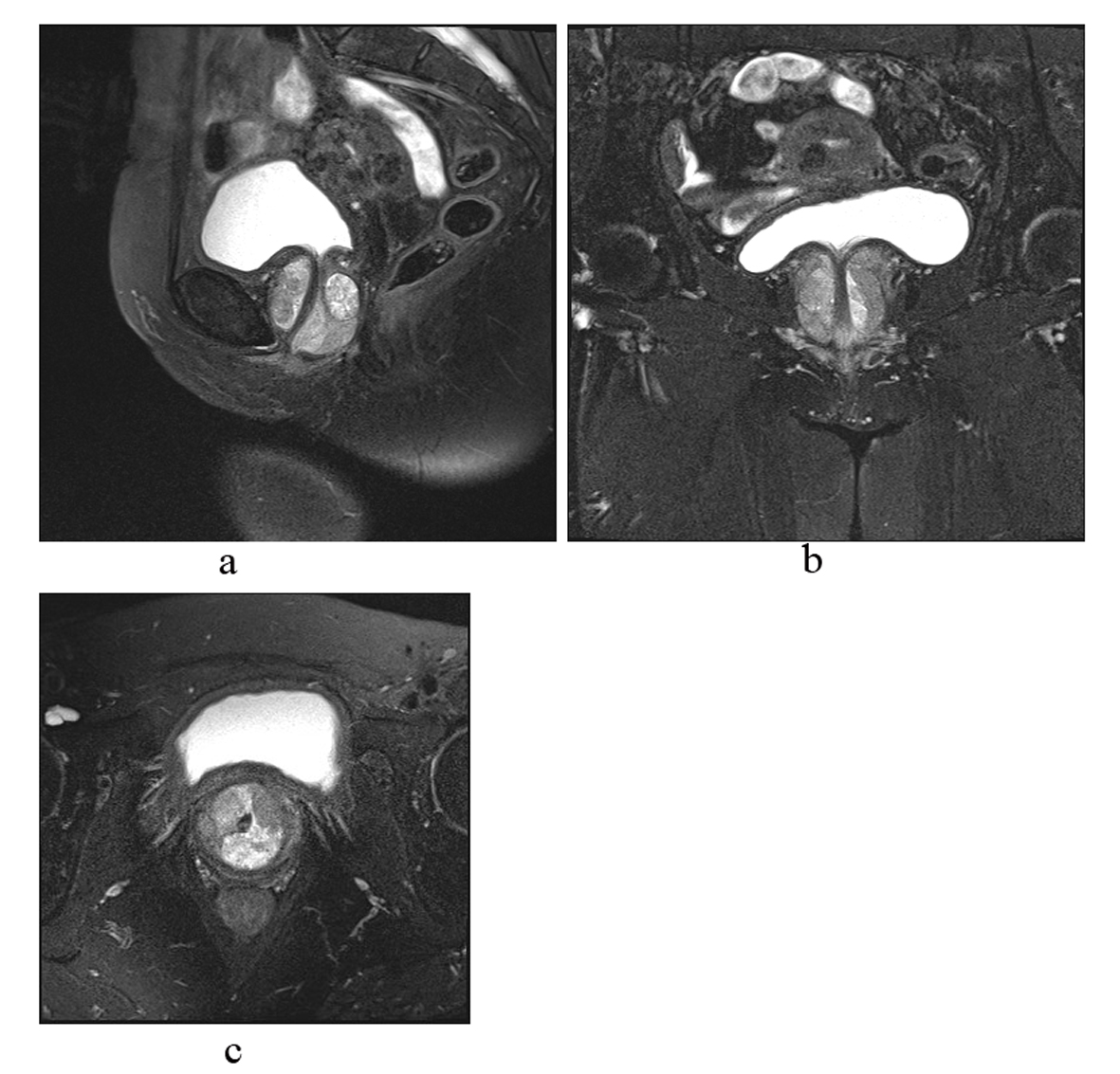 Click for large image | Figure 1. MRI images of heterogenous mass within a urethral diverticulum. |
Histology demonstrated invasive carcinoma with large solid sheets, with round nest-like formations and clearing of the cytoplasm (Fig. 2). There is moderate nuclear pleomorphism with a high number of mitoses. Immunohistochemically cells were positive for: cytokeratin 7 and p16, p53, CA125, CAM5.2, AE1/AE3. They were negative for: thrombomodulin, oestrogen, progesterone, cytokeratin 20, p63, CD10, CEAP, WT1, AFP, s100.
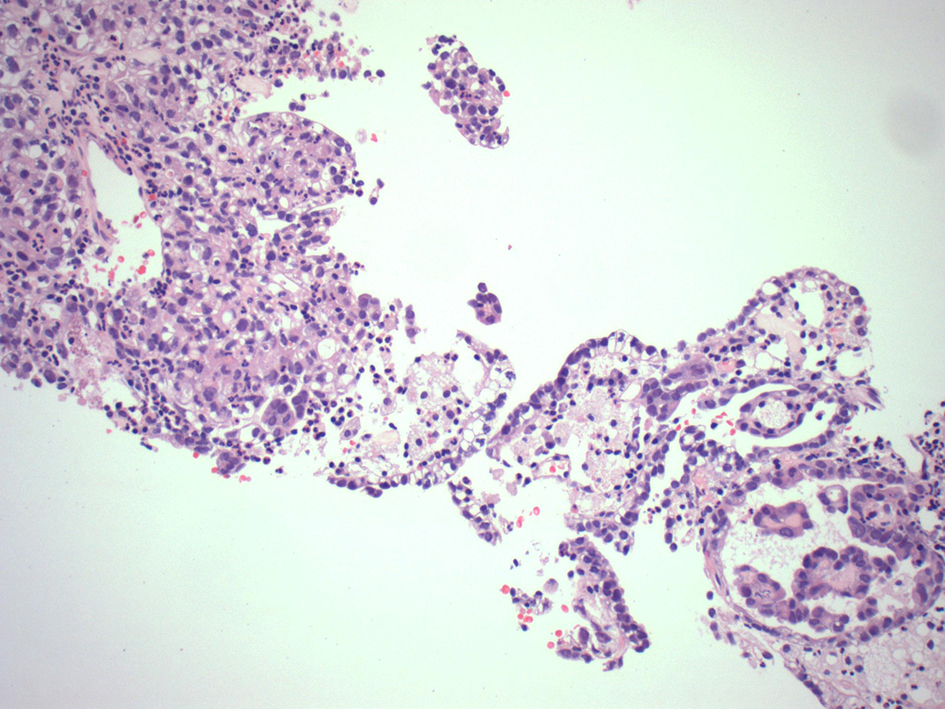 Click for large image | Figure 2. Biopsies showed a combination of clear cell adenocarcinoma of urothelial origin with carcinoma in situ. |
She underwent surgical resection with an anterior exenteration with pelvic lymphadenectomy and ileal conduit formation. Histology showed moderately differentiated CCA of the urethra with invasion into the muscularis propria. Radial margins were clear, however lymphovascular space invasion was present with 3/6 obturator lymph nodes positive for metastases. A multiple disciplinary team decision to offer her only consolidation radiotherapy was based on the existing literature, which has demonstrated a lack of benefit with chemotherapy. She underwent a total of 50.4Gy delivered in 28 fractions to the pelvis: the primary tumour bed and the obturator, sacral and iliac nodal basin.
| Discussion | ▴Top |
Clear cell adenocarcinoma is a rare variant of adenocarcinoma of the urinary tract with approximately 100 case reports to date of which 40 are bladder cases [2, 3]. As mentioned before it was first characterised in 1968 by Dow and Young [1], with the first urethral case in 1973 by Konnak [4]. CCA of the urinary tract has a reported female to male predominance [2]. The median age is 63 and the usual presenting symptoms include hematuria, dysuria, suprapubic pain, retention and urinary tract infections. It is most commonly found at the bladder neck and posterior wall, however is also found at the urethra and trigone. Approximately 50% of urethral cases occur in a urethral diverticulum [5]. Urethral diverticula malignancies were first described in 1951 by Hamilton and Leach [6], with the 100 cases [7, 8] that have been subsequently described the majority have been adenocarcinomas [9, 10].
Pathologically there are three major patterns of CCA: diffuse, papillary and tubulocystic. CCA can have histological variation ranging from flat, cuboidal to a hobnail cell structure, with varying degrees of cytoplasmic clearing, especially eosinophilic/basophilic. There is associated nuclear pleomorphism with necrosis and mitotic activity.
Histogenesis remains controversial with multiple studies describing the origin of CCA ranging from mesonephric, mullerian, nephrogenic or urothelial differentiation. What appears to perpetuate this uncertainty is that CCA is often found with a variety of other tissue forms. For example, our case report found associated urothelial CIS, where as Szymanski [3] reported CCA with surrounding endometriosis. The most recent pathological study by Sung [11] of twelve cases using immunohistochemical and molecular genetic appraisal with fluorescence in situ hybridization reported it to be of urological origin. Their findings included the following: changes in chromosomes 3, 7, 17 as is found with urothelial carcinoma, unlike ovarian which commonly has changes in 1q, identical non-random deactivation of X-chromosome with concurrent urothelial neoplasia. Positivity to CD10 and CK7 occurred at equivalent rates to urothelial carcinoma.
Management principles for CCA are based on expert opinion given the rarity of the disease. Assumptions that urothelial clear cell will behave in a similar fashion to other clear cell malignancies such as cervical cancer have helped guide treatment plans. Despite only having case studies and very small case series [2], it has been shown that surgical resection for localised disease has been curative. Surgical options have ranged from localised transurethral resection (TUR) through to anterior exenteration depending on anatomical considerations with varying success rates.
There is evidence that chemotherapy for more advanced disease provides no survival benefit. Agents used in the past have included cisplatin, doxorubicin, cyclophosphamide, and 5-Fluoruracil [12, 13]. These have only been used in sporadic cases and so it is uncertain whether there are any untried chemotherapy agents which may provide some benefit. The decision to use chemoradiotherapy should be made as part of a multiple disciplinary team approach with the patient fully informed of the risks and benefits. Prognosis is uncertain but based on the limited data available appears to be quite variable, with localised disease having good cure rates, unlike more extensive disease. Progression appears to occur primarily via lymphatic spread.
Clear cell adenocarcinoma of the urinary tract will continue to be a diagnostic and management problem for clinicians given its rarity. Even the uncertainty of its histogenesis: whether this is a single entity or rather a heterogenous collection of different forms of CCA is a question that remains unanswered. This may or may not change management and outcomes. However with the absence of this, treatment at least in the near future will continue to be based on level 4 evidences and as such, patient involvement in the decision process is crucial.
Disclosure
No grant support required. No financial disclosures. Informed consent was obtained, and institutional ethics approval gained.
| References | ▴Top |
- Dow JA, Young JD, Jr. Mesonephric adenocarcinoma of the bladder. J Urol. 1968;100(4):466-469.
pubmed - Lu J, Xu Z, Jiang F, Wang Y, Hou Y, Wang C, Chen Q. Primary clear cell adenocarcinoma of the bladder with recurrence: a case report and literature review. World J Surg Oncol. 2012;10:33.
doi pubmed - Szymanski LJ, Szymanski JM, Muhletaler F, Alassi O. A 50-year-old with gross hematuria. Urology. 2012;80(3):509-511.
doi pubmed - Konnak JW. Mesonephric carcinoma involving the urethra. J Urol. 1973;110(1):76-78.
pubmed - Abascal Junquera JM, Cecchini Rosell L, Martos Calvo R, Salvador Lacambra C, Celma Domenech A, De Torres I, Morote Robles J. [Presentation of a new case of primary clear cell adenocarcinoma of the urethra and its surgical management]. Actas Urol Esp. 2007;31(4):411-416.
doi - Hamilton JD, Leach WB. Adenocarcinoma arising in a diverticulum of the female urethra. AMA Arch Pathol. 1951;51(1):90-98.
pubmed - Nakatsuka S, Taguchi I, Nagatomo T, Yamane M, Sugio K, Yoshino R, Oku K, et al. A case of clear cell adenocarcinoma arising from the urethral diverticulum: Utility of urinary cytology and immunohistochemistry. Cytojournal. 2012;9:11.
doi pubmed - Ha HK, Lee W, Lee SD, Lee JZ, Chung MK. Laparoscopic radical cystourethrectomy in a patient with adenocarcinoma of the female urethral diverticulum. Korean J Urol. 2010;51(2):145-148.
doi pubmed - Clayton M, Siami P, Guinan P. Urethral diverticular carcinoma. Cancer. 1992;70(3):665-670.
doi - Oliva E, Young RH. Clear cell adenocarcinoma of the urethra: a clinicopathologic analysis of 19 cases. Mod Pathol. 1996;9(5):513-520.
pubmed - Sung MT, Zhang S, MacLennan GT, Lopez-Beltran A, Montironi R, Wang M, Tan PH, et al. Histogenesis of clear cell adenocarcinoma in the urinary tract: evidence of urothelial origin. Clin Cancer Res. 2008;14(7):1947-1955.
doi pubmed - Pena Alvarez C, Lorenzo Lorenzo I, Varela Ferreiro S, Pardavila Gomez R, Suh Oh HJ, Saenz de Miera Rodriguez A, Covela Rua M, et al. Clear-cell adenocarcinoma of vesical origin: a case study of metastatic disease treated with chemotherapy. Chemother Res Pract. 2010;2010:426973.
- Kurosaka S, Irie A, Mizoguchi H, Okuno N, Iwabuchi K, Baba S. Advanced clear-cell adenocarcinoma of the bladder successfully treated by radical surgery with adjuvant chemoradiotherapy. Int J Clin Oncol. 2005;10(5):362-365.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
