| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website http://www.wjnu.org |
Case Report
Volume 2, Number 1, June 2013, pages 40-43
Primary Signet-Ring Cell Carcinoma of the Urinary Bladder in an Atomic Bomb Survivor: A Case Report
Kaori Yamashitaa, b, Fumio Itoa, Hayakazu Nakazawaa
aDepartment of Urology, Tokyo Women’s Medical University Medical Center East, 2-1-10, Nishi-ogu, Arakawa-ku, Tokyo, 116-8567, Japan
bCorresponding author: Kaori Yamashita, Department of Urology, Tokyo Women’s Medical University Medical Center East, 2-1-10, Nishi-ogu, Arakawa-ku, Tokyo, 116-8567, Japan
Manuscript accepted for publication May 27, 2013
Short title: Atypical Bladder Tumor
doi: https://doi.org/10.4021/wjnu99w
| Abstract | ▴Top |
Primary signet-ring cell carcinoma of the urinary bladder is a disorder with little detailed information because it has an extremely low incidence and an unfavorable prognosis. We report the case of an 80-year-old male patient with primary signet-ring carcinoma of the bladder. The patient was a long-lived atomic bomb survivor of Hiroshima. He complained of asymptomatic gross hematuria while under successful endocrine treatment for organ-confined prostate cancer. Magnetic resonance imaging showed diffuse thickening of the urinary bladder. Pathological specimens revealed an infiltrating growth of neoplastic cells with a signet-ring cell configuration. The oral administration of tegafur-uracil (200 mg/m2 per day) was initiated; however, the effect of this treatment was temporary. Fourteen months after the start of this treatment, the tumor had involved the bilateral intramural ureters and postrenal azotemia occurred because of bilateral hydronephrosis. Whether the prevalence of signet-ring cell carcinoma in the genitourinary tract is higher in atomic bomb survivors than in the general population remains much debated. The development of this rare and peculiar urothelial cancer after exposure to atomic bombing may give hints to the carcinogenic effect of ionizing radiation.
Keywords: Atomic bomb survivor; Signet-ring cell carcinoma; Urinary bladder
| Introduction | ▴Top |
In this article, we report a case of primary signet-ring cell carcinoma (SRCC) of the urinary bladder. It is an extremely rare high-grade, life-threatening urothelial cancer with a poor prognosis. The importance of this case is the fact that the patient was a long-lived Hiroshima atomic bomb survivor, and his tumor had an extremely rare manifestation as a primary bladder neoplasm.
The Radiation Effects Research Foundation reports that carcinomas of the urinary tract, including the bladder, have a high excess relative risk as a major cause of death among Hiroshima and Nagasaki atomic bomb survivors [1]. In gastric cancer, poorly differentiated adenocarcinoma and SRCC are higher in Hiroshima atomic bomb survivors [2]. However, it is unclear whether the number of cases of high-grade urothelial cancers including SRCC is greater than the number of cases of low-grade urothelial cancer in atomic bomb survivors, in addition, it is not obvious whether exposure to ionizing radiation affects the pathological change. To resolve this problem, the reports of every patient with exposure to ionizing radiation and who are diagnosed with urothelial cancer will be needed. Therefore, we present the clinical course of our patient and discuss problems with other reports in the literature.
| Case Report | ▴Top |
A 79-year-old Japanese man was referred to our department because of an elevated serum prostate-specific antigen (PSA) value. He had no past medical history, except for radiation exposure from an atomic bombing. When the atomic bomb was detonated over Hiroshima on August 6, 1945, he was within a wooden construction located 1.7 km from ground zero and exposed to about 0.072 Gy of ionizing radiation as DS02 urinary bladder organ dose [3]. He was diagnosed with stage pT2bN0M0 prostate cancer. A pathology examination showed a moderately differentiated adenocarcinoma. His Gleason score was 4 + 3 = 7. He underwent combined androgen blockade therapy. One year after initiating this therapy, asymptomatic gross hematuria was present, although his serum PSA value had already fallen below the detectable limit. Magnetic resonance imaging depicted diffuse thickening of the urinary bladder (Fig. 1). Cystoscopy showed that multiple sessile tumors had developed from the posterior and bilateral walls of the bladder. A pathological analysis of the biopsy specimens revealed that tumor cells had infiltrated from the mucosa into the lamina propria. The cells were crescent-shaped with their nuclei compressed to one edge and a vacuole (Fig. 2). Further examinations, which included gastrointestinal fiberscopy, ruled out the possibility of SRCC of the gastrointestinal tract. Therefore, the tumor was diagnosed as being of bladder origin. The tumor was organ-confined at that time. However, he refused any excessive therapy such as intravenous anticancer chemotherapy or cystectomy because of his advanced age. The oral administration of tegafur-uracil (200 mg/m2 per day) was initiated. Six months later, his serum CA 19-9 value - which is a reliable test for SRCC activity - had declined to 35.8 U/mL from 42.9 U/mL (The normal range is less than 37 U/mL). However, 12 months after the start of this treatment, his CA 19-9 value gradually increased and finally reached 109.7 U/mL. He had severe normocytic and normochromic anemia and rapid deterioration of renal function. Computed tomography (CT) demonstrated that the distal ends of both ureters were involved in the tumor, which had infiltrated the whole bladder and resulted in postrenal azotemia. A percutaneous nephrostomy was immediately placed in the right renal pelvis. He was administered palliative care. He died in March 2013 because of cancerous cachexia.
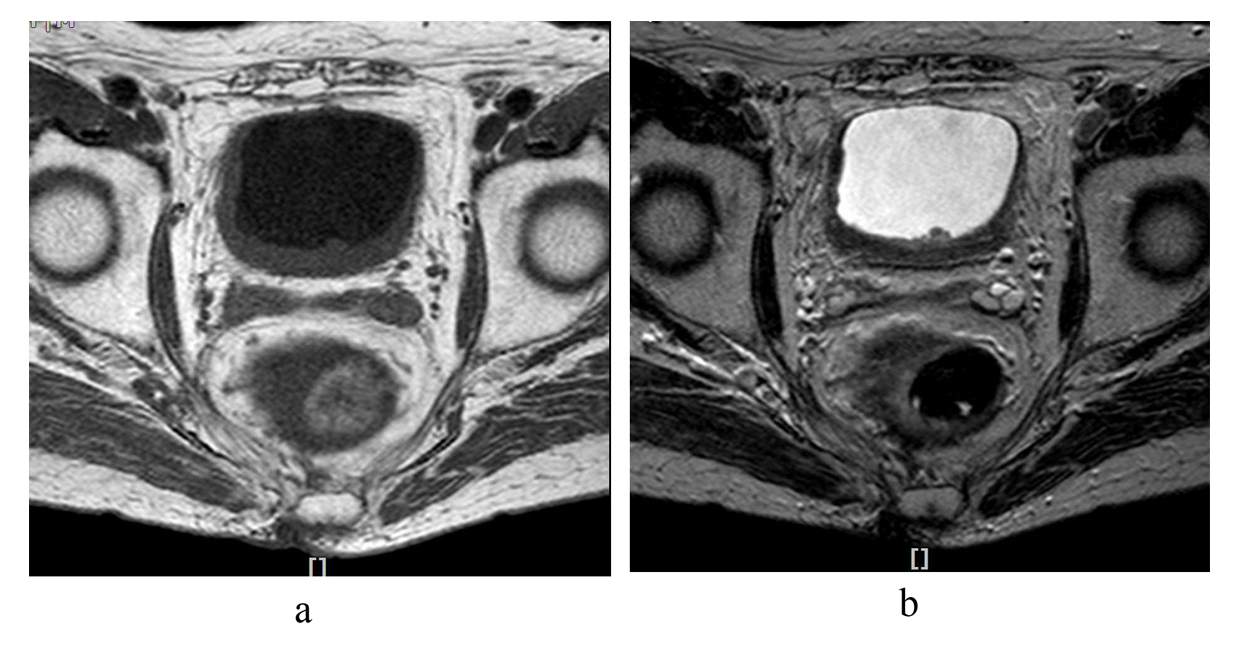 Click for large image | Figure 1. (a). T1- and (b). T2-weighted magnetic resonance imaging shows thickening of the posterior and bilateral walls of the bladder. |
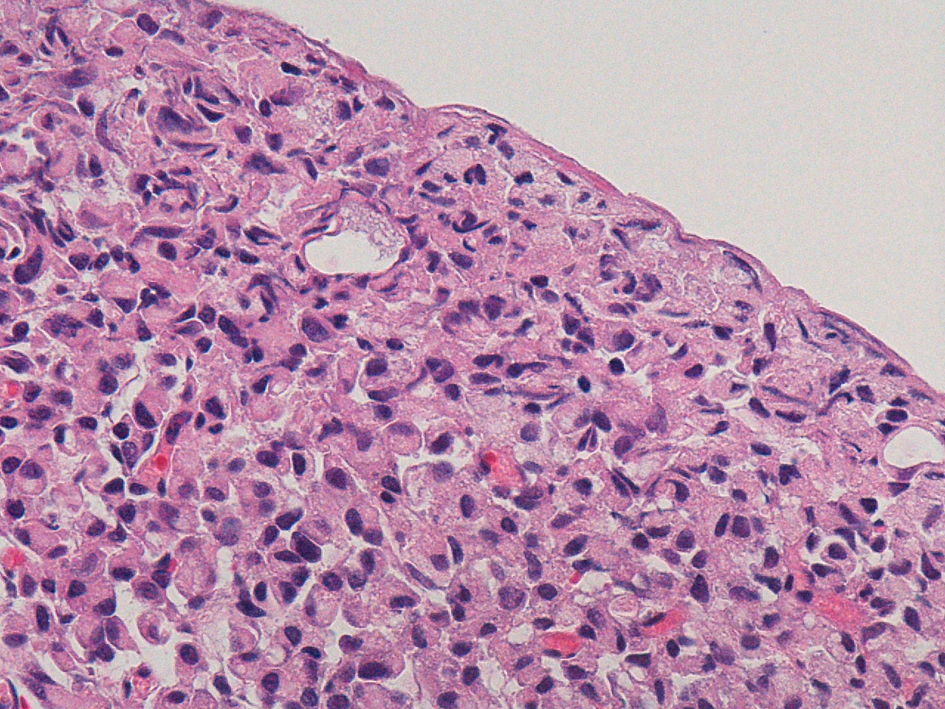 Click for large image | Figure 2. The pathological specimen shows diffuse infiltration of signet-ring cells (hematoxylin and eosin stain; magnification, 400 ×). |
| Discussion | ▴Top |
Adenocarcinomas account for less than 2% of primary bladder cancers [4]. Signet-ring cell carcinoma is classified as an adenocarcinoma and is extremely rare. To our knowledge, there are 56 reported cases. Our patient is the 57th case reported in Japan. Wang et al [5] report that a study of 198,317 patients with primary bladder cancer revealed 230 (0.12%) cases of SRCC.
In histogenesis, Kunze et al [6] found pS2 peptide and MUC5AC mucin in primary adenocarcinoma and in SRCC of the urinary bladder. Since the expression of both proteins was absent in the normal nonneoplastic urothelium, their appearance in association with the tumor was regarded as a neoexpression or as a re-expression. This evidence supported the concept that adenocarcinomas, including SRCC, may histogenetically develop from preexistent transitional cell carcinomas.
Most patients with SRCC tend to be diagnosed at an advanced stage at their first visit because pathologic signet-ring cells first invade the mucosa and submucosa of a hollow organ with eventual full-thickness involvement [7, 8]. Therefore, CT or magnetic resonance imaging (MRI) may detect SRCC as a thickened bladder wall. Partial or radical cystectomy has been selected as a curative treatment for patients who are younger at the time of their SRCC diagnosis [5, 9].
Our patient reserved authorization of atomic bomb disease because he was within 3.0 km from ground zero in Hiroshima when the atomic bomb was detonated. Atomic bomb disease is known to later become prostatic cancer or urothelial carcinoma because of ionizing radiation. The Radiation Effects Research Foundation reports that in the Life Span Study of atomic bomb survivors, cohort members who received doses greater than 0.005 Gyw (average dose of 0.21 Gyw), the attributable fraction of urothelial carcinoma resulting from radiation was 7.1% in males and 19.7% in females [10]. In studies on the mortality of atomic bomb survivors, the excess relative risk per Gy (ERR/Gy) of all solid cancers was 0.47 (95% confidence interval (CI), 0.38 - 0.56). However, the ERR/Gy of bladder cancer was 1.12 (95% CI, 0.33 - 2.26) in particular, the ERR/Gy of the renal pelvis and ureter was 2.62 (95% CI is 0.47 - 7.25) [1].
Smoking is a factor that influences urothelical carcinoma. This patient was a heavy smoker and had smoked forty cigarettes daily for 55 years. During a lifespan study of atomic bomb survivors, Grant et al [10] reported the effects of radiation and lifestyle factors (for example, smoking; consumption of fruit, vegetables, alcohol; and education level) on the risk of developing urothelial carcinoma. Grant concluded that smoking was the primary factor responsible for excess urothelial carcinoma in their cohort study, but smoking did not appear to strongly confound or modify the radiation risk estimates of urothelial carcinoma.
The Radiation Effects Research Foundation reports that, among atomic bomb survivors, bladder cancer, stomach cancer, lung cancer, liver cancer, colon cancer, breast cancer, gall bladder cancer, esophageal cancer, and ovarian cancer show a significant increase of cancer mortality because of radiation [1]. The number of patients with gastric cancer is larger than the number of patients with urothelial cancer. Signet-ring cell carcinoma gastric cancer is not rare. In a study of the histology of stomach cancer in atomic bomb survivors, poorly differentiated adenocarcinoma (namely, poorly differentiated adenocarcinoma and SRCC) is significantly higher in people receiving 1 rad (0.01 Gy) or more than in people receiving 0 rad [2]. However, there are few studies on the relationship between radiation exposure and the histological type of urothelial carcinoma. The pathological specimens from our patient did not reveal conventional urothelial carcinoma. This led us to speculate that a relationship exists between high-grade urothelial carcinoma and ionizing radiation. We believe that there may be some cases of high-grade carcinoma, including SRCC, in atomic bomb survivors with urothelial carcinoma. Because the mortality of urothelial carcinoma in atomic bomb survivors is higher than the mortality of other solid cancers, SRCC is a high-grade and life-threatening carcinoma with a poor prognosis.
Morimura et al [11] report that the incidence of urinary bladder in the Ukraine increased gradually from 26.2 to 43.3 per 100,000 people between 1986 and 2001 after the Chernobyl accident. The Morimura group also demonstrated an increased incidence of bladder dysplasia and/or bladder cancer, including carcinoma in situ, that is accompanied by an increased cesium 137 (Cs137) level in urine among people living in the radio contaminated area. Morimura showed that a distinct molecular pathway may exist in the genesis of bladder cancer, based on the specific etiology.
In Japan, The Fukushima Daiichi nuclear disaster occurred after the Tohoku earthquake and tsunami on March 11, 2011. The nuclear disaster resulted in a series of equipment failure, nuclear meltdown, and the release of radioactive materials at the Fukushima I Nuclear Power Plant. It is the largest nuclear disaster since the Chernobyl disaster of 1986. It measured level 7 on the International Nuclear Event Scale. The number of patients with urothelial carcinoma may increase in this area. We recommend taking into account information concerning the life, occupation, and residential history of patients with high-grade urothelial carcinoma in the long term. It may contribute to the discovery of new carcinogenic pathways of urothelial carcinoma resulting from ionizing radiation effect.
In conclusion, we report a case of primary SRCC of the urinary bladder in an atomic bomb survivor. The relationship between the histological type of urothelial carcinoma and the ionizing radiation effect remains unclear. To solve this problem will require an examination of all reports of patients exposed to ionizing radiation and diagnosed with urothelial cancer.
Acknowledgments
The authors have no conflict of interests to report.
Support Information
None.
| References | ▴Top |
- Ozawa K, Shimizu Y, Suyama A, Kasagi F, Soda M, Grant EJ, Sakata R, et al. Studies of the mortality of atomic bomb suivivors, report 14 1950-2003 : an overview of cancer and noncancer diseases. Diseases. Radiat. Res. 2012; 177: 229-243.
doi pubmed - Ito C, Kato M, Yamamoto T, Ota N, Okuhara T, Mabuchi K, Otake M, et al. Study of stomach cancer in atomic bomb survivors. Report 1. Histological findings and prognosis. J Radiat Res. 1989;30(2):164-175.
doi pubmed - Young RW, Kerr GD. Reassessment of the Atomic Bomb Radiation Dosimetry for Hiroshima and Nagasaki. Japan : The Radiation Effects Research Foundation, 2005:1-13.
- Wood DP. Urothelial Tumors of the bladder: Urothelial cancer: Pathology. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA (eds). Campbell-Walsh UROLOGY, ed. Saunders, Philadelphia, 2012; 2316-2323.
doi - Wang J, Wang FW. Clinical characteristics and outcomes of patients with primary signet-ring cell carcinoma of the urinary bladder. Urol Int. 2011;86(4):453-460.
doi pubmed - Kunze E, Krassenkova I, Fayyazi A. Tumor-associated neoexpression of the pS2 peptide and MUC5AC mucin in primary adenocarcinomas and signet ring cell carcinomas of the urinary bladder. Histol Histopathol. 2008;23(5):539-548.
pubmed - Ohtsuki Y, Fukumoto T, Okada Y, Teratani Y, Hayashi Y, Lee GH, Furihata M. Immunohistochemical and ultrastructural characterization of the signet-ring cell carcinoma component in a case of urothelial carcinoma of the urinary bladder. Med Mol Morphol. 2010;43(2):96-101.
doi pubmed - Lane Z, Hansel DE, Epstein JI. Immunohistochemical expression of prostatic antigens in adenocarcinoma and villous adenoma of the urinary bladder. Am J Surg Pathol. 2008;32(9):1322-1326.
doi pubmed - Shringarpure SS, Thachil JV, Raja T, Mani R. A case of signet ring cell adenocarcinoma of the bladder with spontaneous urinary extravasation. Indian J Urol. 2011;27(3):401-403.
doi pubmed - Grant EJ, Ozasa K, Preston DL, Suyama A, Shimizu Y, Sakata R, Sugiyama H, et al. Effects of radiation and lifestyle factors on risks of urothelial carcinoma in the Life Span Study of atomic bomb survivors. Radiat Res. 2012;178(1):86-98.
doi pubmed - Morimura K, Romanenko A, Min W, Salim EI, Kinoshita A, Wanibuchi H, Vozianov A, et al. Possible distinct molecular carcinogenic pathways for bladder cancer in Ukraine, before and after the Chernobyl disaster. Oncol Rep. 2004;11(4):881-886.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
