| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website https://www.wjnu.org |
Original Article
Volume 13, Number 1, July 2024, pages 13-18
Clinical Utiliy of Routine Postoperative Laboratory Tests After Laparoscopic Prostate Surgery
Bernardo Lobao Teixeiraa, b , Joao Ferreira Cabrala
, Avelino Fragaa
aUrology Department, Centro Hospitalar Universitario de Santo Antonio, Porto, Portugal
bCorresponding Author: Bernardo Lobao Teixeira, Department of Urology, Centro Hospitalar Universitario de Santo Antonio, Porto, Portugal
Manuscript submitted August 12, 2023, accepted September 20, 2023, published online November 21, 2023
Short title: Laboratory Tests After Laparoscopic Prostate Surgery
doi: https://doi.org/10.14740/wjnu444
| Abstract | ▴Top |
Background: Post-operative protocols, including blood tests, are frequently implemented to standardize care and as guarantees of safety before discharge. They might however be unnecessary after minimally invasive surgery. Our objective was to determine the clinical utility of routine postoperative blood test after laparoscopic prostate surgery.
Methods: A retrospective review of 231 patients who underwent laparoscopic prostatectomy was conducted. The primary outcome was the rate of clinically significant blood loss, defined as a drop in hemoglobin level of 4 g/dL or the need for a blood transfusion. A logistic regression model was developed for the outcomes of interest.
Results: Final review included 231 patients. Forty-five patients (19.5%) had at least one abnormal blood test parameter on the first post-operative day. Eleven patients (4.8%) had clinically significant blood loss, with four patients (1.7%) overall requiring a blood transfusion. All patients requiring a transfusion had a significant complication that was clinically evident; all other abnormal blood tests were mild and did not change routine care. Signs of hemodynamic instability were the main predictors of clinically significant blood loss on multivariable regression analysis, with an odds ratio (OR) of 4.14 (95% confidence interval (CI): 1.12 - 15.35; P = 0.034).
Conclusions: Routine post-operative blood tests have low yield, seldomly changing care. Signs of hemodynamic instability were the main predictors of significant blood loss and can be used as triggers for laboratory testing. Reducing routine laboratory tests improves patients’ experience, diminishes cost and hospital stay. Our results provide evidence to perform radical prostatectomies in a 1-day surgery setting.
Keywords: Prostatectomy; Laparoscopy; Diagnostic tests; Blood loss; Surgical
| Introduction | ▴Top |
Prostate cancer is the second most frequent cancer worldwide, and the fifth leading cause of cancer death in men [1]. Likewise benign prostatic hyperplasia (BPH) is highly prevalent, with rates of 36-44% or higher [2, 3]. Unsurprisingly, such high incidence and prevalence has led to an increased number of prostate surgeries over the years [4].
It is not uncommon for surgical departments to develop post-operative protocols to standardize and optimize care, increase reproducibility between physicians and nursing staff, and guarantee patient safety before discharge. Such protocols frequently include blood tests on the first day following surgery in order to screen for significant bleeding, organ dysfunction or electrolyte imbalances. Recent studies have observed a decreased need of blood transfusions after surgery (7% to 5%), in relation to the increased use of minimally invasive techniques and more restrictive transfusion practices [5]. As a result, routine post-operative blood tests might not be useful or cost-effective and could be avoided.
The objective of the current study was to assess the need of routine postoperative blood tests after laparoscopic prostatic surgery and to tailor such exams to specific clinical situations.
| Materials and Methods | ▴Top |
Study design
We designed a retrospective study including consecutive patients admitted for simple or radical laparoscopic prostatectomy at our institution, an academic university hospital, between January 2017 and December 2019. Procedures were either performed by a senior urologist with extensive experience in laparoscopic surgery or by a resident tutored by the assistant. Both procedures were performed in an extraperitoneal fashion, through five laparoscopic ports, similar to the initial technique described for laparoscopic radical prostatectomy [6]. A surgical drain was left in place after all procedures. Patients were discharged to the urology ward after the post-anesthesia care unit and started ambulation and liquid diet the following morning. Department protocol mandates routine postoperative laboratory blood tests and ambulation on post-operative day 1. Parameters analyzed included a complete blood count (CBC), creatinine (Cr), urea (U), sodium (Na), potassium (K) and chloride (Cl). Surgical drain is removed once output is lower than 50 cc after ambulation, and the patient is usually discharged on the day following its removal.
Patients without post-operative laboratory results were excluded. The patient flow diagram is displayed in Figure 1. Sixteen patients had missing variables, as summarized in the figure.
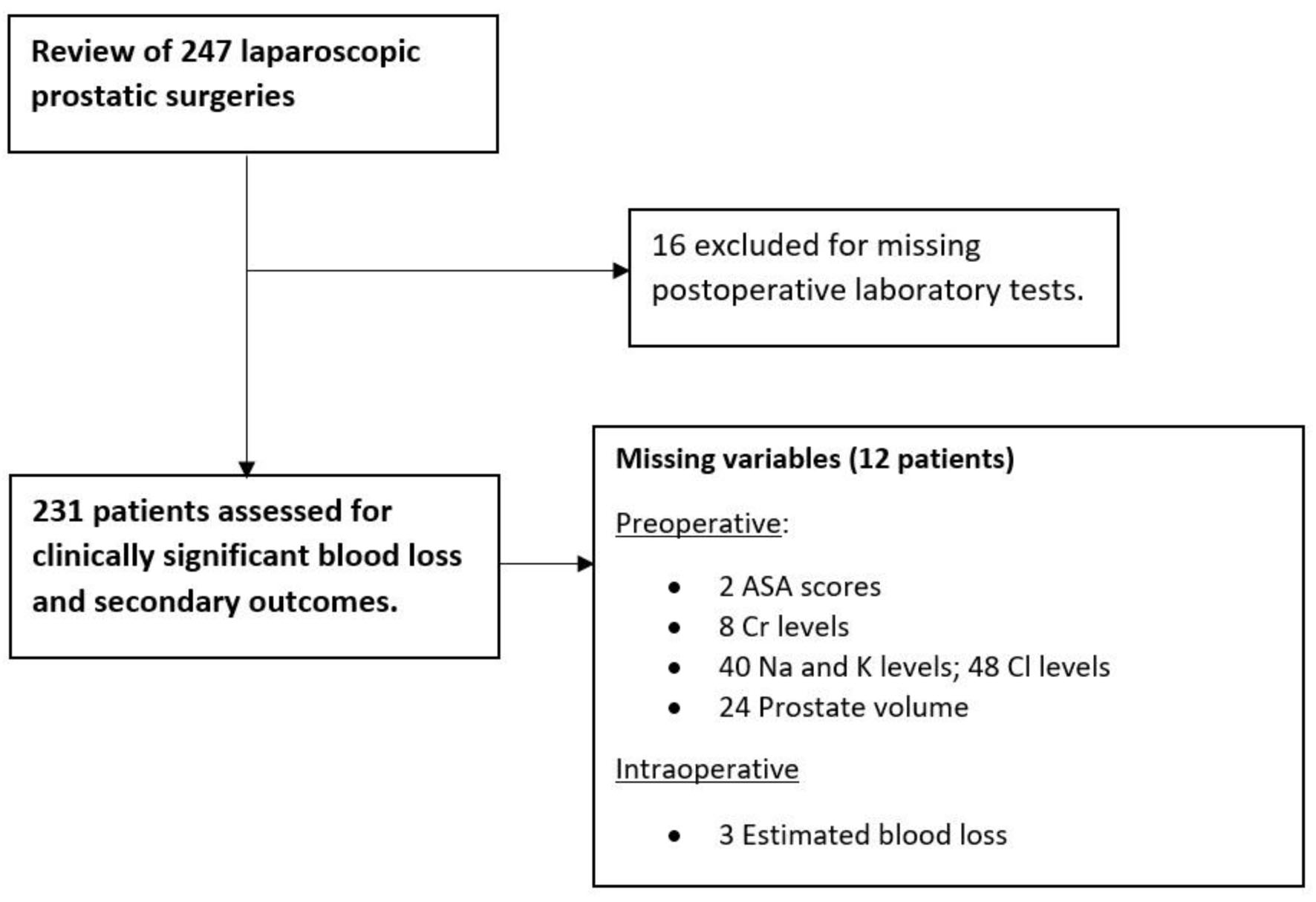 Click for large image | Figure 1. Patient flow diagram. |
Local ethics committee approved the study and waived the need for informed consent. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Definitions and variables
Data were collected on patient characteristics (age, body max index (BMI), American Society of Anesthesiology (ASA) score, chronic use of antiplatelet or anticoagulants, prostate volume measured by transrectal or suprapubic ultrasound), intraoperative information (total operative time, estimated blood loss), post-operative information (length of stay, readmission rate, transfusion rate, complications as graded by Clavien-Dindo within 90 days of discharge, drain output and clinical signs of hemodynamic instability, namely, tachycardia (more than 100 bpm) and hypotension (systolic blood pressure lower than 100 mmHg)) and preoperative and postoperative (first day post-surgery) laboratory values (hemoglobin, serum creatinine, sodium, potassium and chloride). Preoperative laboratory tests were collected up to 6 months before surgery. Abnormal hemoglobin was defined as a fall in hemoglobin level equal to or higher than 4 g/dL or need for blood transfusion. Use of this cut-off was based on the methodoloy of a study addressing the contemporary management of hemorrhage after minimally invasive radical prostatectomy [7]. Abnormal lab values were defined by local laboratory reporting parameters. Acute kidney injury was defined according to the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines as were chronic kidney disease stages. Glomerular filtration rate was calculated using Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation.
Outcomes
The primary outcome of interest was clinically significant blood loss, which we defined as either a fall in hemoglobin level of 4 g/dL or need for blood transfusion. Secondary outcome was the rate of abnormal blood tests (clinically significant blood loss, electrolyte disturbance or acute kidney injury).
Statistical analysis
Data were analyzed using IBM SPSS Statistics v.26®. Univariable regression analysis included variables of interest for clinically significant blood loss and abnormal post-operative blood tests. Statistically significant predictors on univariate analysis were included in a multivariable logistic regression model for both outcomes.
Odds ratios (ORs) were reported with 95% confidence intervals (CIs). Statistical significance was considered at a P-value of < 0.05.
| Results | ▴Top |
Table 1 provides a summary of patients’ characteristics, intraoperative, and post-operative information. Final analysis included 231 patients after excluding patients with missing post-operative hemoglobin measurment. Eleven (4.8%) patients overall experienced clinically significant blood loss (7 (3%) after simple prostatectomy and four (1.7%) after radical prostatectomy), with four (1.7%) of them requiring a blood transfusion, including one (0.4%) in the radical prostatectomy cohort and three (1.3%) in the simple prostatectomy group.
 Click to view | Table 1. Demographic and Baseline Data |
Forty-five patients (19.5%) had at least one abnormal blood test parameter on the first postoperative day, which included the 11 patients with clinically significant blood loss mentioned earlier. Additionally, 22 patients (9.5%) had postoperative Cr levels above 1.2 mg/dL, indicating that five patients (2.2%) experienced an acute kidney injury stage 1 according to the KDIGO definition. Furthermore, 16 (6.8%) patients had mild changes in their sodium or chloride levels, reflecting electrolyte imbalances. None of them was significant enough to require aditional treatment.
Table 2 presents the results of the univariate analysis, exploring the variables of interest and their associations with clinically significant blood loss and abnormal laboratory values on the first postoperative day. Simple prostatectomy showed an increased risk of clinically significant blood loss compared to radical prostatectomy in the univariate analysis, with an OR of 3.93 (95% CI: 1.11 - 13.87, P = 0.03). Intraoperative estimated blood loss and clinical signs of hemodynamic instability were also significantly associated with clinically significant blood loss, with ORs of 1.00 (95% CI: 1.00 - 1.005, P = 0.021) and 4.19 (95% CI: 1.18 - 14.79, P = 0.026), respectively.
 Click to view | Table 2. Univariable Analysis for Clinically Significant Blood Loss and Abnormal Blood Test Result on Day 1 Post Prostatectomy |
Regarding abnormal laboratory values on postoperative day 1, the univariate analysis identified significant predictors: type of surgery, with an OR of 2.69 for simple prostatectomy (95% CI: 1.38 - 5.25; P = 0.004), ASA score, with an OR of 3.09 (95% CI: 1.49 - 6.45; P = 0.002), and antiplatelet or anticoagulant medication, with an OR of 2.17 (95% CI: 1.04 - 4.54; P = 0.04).
Next, we further investigated the variables associated with the outcomes of interest using multivariable logistic regression analysis (Table 3). Signs of hemodynamic instability remained the primary predictor of clinically significant blood loss, with an OR of 4.14 (95% CI: 1.12 - 15.35; P = 0.034). Additionally, both ASA score (OR: 2.40, 95% CI: 1.10 - 5.24; P = 0.029) and simple prostatectomy (OR: 2.25, 95% CI: 1.13 - 4.48; P = 0.022) were associated with abnormal laboratory test results on post-operative day 1.
 Click to view | Table 3. Multivariable Analysis for Clinically Significant Blood Loss and Abnormal Blood Rest Result on Day 1 Post Prostatectomy |
| Discussion | ▴Top |
Open prostatic surgery has long been associated with extended hospital stays and perioperative complications. Over time, technical advancements have been made to improve the procedures. Despite these efforts, some series still report hospital stays of 6 to 12 days and transfusion rates of 7.5% to 12.7% for simple open prostatectomy, and 3 days and 30% for open radical prostatectomy [8-10]. To address these challenges, minimally invasive surgery has been globally implemented, leading to better outcomes. Our study adds to the existing literature, supporting the benefits of laparoscopic approaches, which show reduced blood loss and shorter hospital stays [11, 12].
In our cohort, routine blood tests were of no clinical interest after laparoscopic surgery. Although almost 20% of patients had abnormal results on the first day after surgery, they did not lead to meaningful changes in patient care or outcomes. Patients who did develop significant complications during the post-operative period could promptly be identified based on surgical reports and clinical examinations alone, and this was further corroborated by multivariable analysis, where signs of hemodynamic instability were the main predictors of blood loss. Among the patients who required a blood transfusion, we encountered four distinct cases. In one patient undergoing radical prostatectomy, a peritonitis occurred due to an unnoticed rectal laceration, necessitating a laparotomy with a terminal colostomy. In the simple prostatectomy group, one patient received a late diagnosis of acquired hemophilia. Another patient experienced a myocardial infarction during surgery, leading to transfer to a cardiac intensive care unit and the initiation of antiplatelet medication. Lastly, the fourth patient received a transfusion due to symptomatic anemia, as their preoperative hemoglobin level was 10 g/dL and dropped to 8 g/dL. We argue that any of these cases would intuitively be detected based on the overall clinical scenario, and not because of routine blood tests after surgery.
Drain output showed no significant correlation with significant blood loss, which may be attributed to low drainage levels in the majority of patients. Our analysis suggests that intraoperative blood loss is a stronger predictor of significant blood loss, supported by both univariable and multivariable analyses. Interestingly, while surgical drains after radical prostatectomy are commonly used in many centers, evidence from randomized control trials indicates that a no-drain policy is non-inferior to using a drain after the procedure [13]. In a retrospective analysis by Chestnut et al involving over 3,000 patients who underwent minimally invasive radical prostatectomy (laparoscopic or robot-assisted) between 2010 and 2018, despite a low transfusion rate of 1.2%, routine post-operative assessment of hemoglobin persisted at their institution, possibly influenced by practices from the era of open surgery [14]. Consistent with our findings, they also concluded that signs and symptoms of hemodynamic instability were the primary drivers for transfusions, rather than absolute hemoglobin levels. While their study focused on patients undergoing radical prostatectomy, our results extend these findings to minimally invasive prostatectomy in the context of benign prostatic hyperplasia (BPH). Interestingly, the latter procedure demonstrated a higher transfusion rate and increased risk of significant post-operative bleeding, possibly associated with prostatic fossa bleeding, which required irrigation after surgery.
Our study strongly supports utilizing hemodynamic status as a trigger for closer postoperative follow-up and blood testing. While more than 30% of patients showed signs of hemodynamic instability, only 4.8% experienced clinically significant blood loss. The discrepancy in values between this variable and the outcome could be related to how it is measured and the imperfect correlation between the two. For instance, a patient with a single measurement of a heart rate of 101 bpm might be classified as “hemodynamically unstable”, despite being otherwise well and asymptomatic. However, this gap provides a crucial safety margin for avoiding unnecessary blood tests while ensuring prompt identification and intervention for patients at risk of clinically significant blood loss.
Healthcare costs have been rising in many Organization for Economic Co-operation and Development (OECD) countries due to the increased burden of diseases in an aging population [15]. One contributing factor to these costs is the excessive use of unnecessary laboratory testing, which adds financial strain without providing any clinical benefits. At our institution, we have observed that routine post-operative blood tests for laparoscopic prostatectomies cost approximately €7 per patient. A conservative analysis based on our cohort would mean that €268 could be saved directly every year by avoiding routine blood tests in the close to 70% of patients without any sign of hemodynamic instability. Additionally, delayed reporting of blood tests and missed venepunctures often lead to unnecessary delays in discharging otherwise stable patients. To put this into perspective, the median cost per patient-day on our ward is €581.60. By reducing the hospital stay by just 1 day for 70% of laparoscopic radical prostatectomies (37 procedures per year), we could save around €21,519 annually. However, such reasoning may not directly apply to the simple prostatectomy group, as their prolonged discharge may be related to factors other than delayed blood test reporting, such as the need for bladder irrigation or specific protocol variations. Moreover, when considering our radical prostatectomy cohort’s median hospital stay (median 3 days, interquartile range (IQR) 3 - 4), various factors related to our protocol, besides delayed reporting of blood tests, might contribute to a prolonged hospital stay.
It is essential to consider the risks associated with venipunctures, including the potential for hematomas or phlebitis in patients and accidental punctures in healthcare professionals. These procedures also cause unnecessary pain and anxiety for patients as they await results. To address this, Nathan et al successfully reduced post-operative blood tests by 73% after robotic-assisted radical prostatectomy by issuing specific recommendations based solely on intra- and post-operative clinical findings [16].
Given the low complication rate and the limited utility of routine post-operative blood tests after minimally invasive radical prostatectomy, the focus should be on transitioning towards ambulatory settings [17, 18]. While the idea of strict outpatient radical prostatectomies may seem ambitious, it is worth noting that more than 50% of patients initially planned for outpatient robotic-assisted radical prostatectomies ultimately required overnight stays [19]. Therefore, a more feasible approach is aiming to discharge patients within 23 h. Alvin et al demonstrated the success of this strategy, reporting a remarkable 97% of patients discharged within 23 h after surgery in an ambulatory extended recovery setting [18].
Several limitations should be considered in our study. Firstly, as a retrospective study, inherent biases may exist. Secondly, it is important to note that most procedures in our cohort were performed or mentored by highly experienced laparoscopic surgeons, so the findings may not fully apply to surgeons who are still on the learning curve for radical or simple laparoscopic prostatectomy. Regarding the analysis of potential hemodynamic instability, we primarily relied on clinical signs such as blood pressure and heart rate, which simplifies the assessment of physiologic homeostasis. We did not include an analysis of patients’ symptoms or other indicators like urinary output, which could be relevant in identifying patients who require closer follow-up.
Despite these limitations, it is unlikely that we missed important clinical outcomes due to the low incidence of serious complications observed during our follow-up period.
Lastly, our brief cost analysis may have some over- or underestimations, and direct comparisons with other centers may not be entirely applicable due to variations in costs across hospitals and health systems.
Conclusions
Based on our findings, routine post-operative laboratory tests following laparoscopic simple or radical prostatectomy should be reconsidered, as they offer little clinical relevance and contribute to increased healthcare costs without providing additional benefits to patients. Instead, our study highlights the value of relying on intraoperative and clinical data, which appear to be sufficient for predicting significant blood loss after surgery in light of an overall low incidence of perioperative complications. Embracing this approach can optimize healthcare resources while maintaining high-quality patient care standards.
Acknowledgments
None to declare.
Financial Disclosure
No funding was obtained for the current study.
Conflict of Interest
The authors have no conflict of interest to report.
Informed Consent
Need for informed consent was waived.
Author Contributions
Bernardo Lobao Teixeira: study design, data acquisition, statistical analysis and manuscript writing. Joao Ferreira Cabral: study design and manuscript revision. Avelino Fraga: study design, study oversight, and manuscript revision.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Garg V, Byrom I, Agnew N, Starks I, Phillips S, Malek IA. Routine postoperative blood tests in all patients undergoing Total Hip Arthroplasty as part of an enhanced recovery pathway: Are they necessary? J Clin Orthop Trauma. 2021;16:114-118.
doi pubmed pmc - Bosch JL, Hop WC, Kirkels WJ, Schroder FH. The International Prostate Symptom Score in a community-based sample of men between 55 and 74 years of age: prevalence and correlation of symptoms with age, prostate volume, flow rate and residual urine volume. Br J Urol. 1995;75(5):622-630.
doi pubmed - Chute CG, Panser LA, Girman CJ, Oesterling JE, Guess HA, Jacobsen SJ, Lieber MM. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993;150(1):85-89.
doi pubmed - Jegerlehner S, Chiolero A, Aujesky D, Rodondi N, Germann S, Konzelmann I, Bulliard JL, et al. Recent incidence and surgery trends for prostate cancer: Towards an attenuation of overdiagnosis and overtreatment? PLoS One. 2019;14(2):e0210434.
doi pubmed pmc - Nordestgaard AT, Rasmussen LS, Sillesen M, Steinmetz J, Eid AI, Meier K, Kaafarani HMA, et al. Red blood cell transfusion in surgery: an observational study of the trends in the USA from 2011 to 2016. Anaesthesia. 2020;75(4):455-463.
doi pubmed - Schuessler WW, Schulam PG, Clayman RV, Kavoussi LR. Laparoscopic radical prostatectomy: initial short-term experience. Urology. 1997;50(6):854-857.
doi pubmed - Dean LW, Tin AL, Chesnut GT, Assel M, LaDuke E, Fromkin J, Vargas HA, et al. Contemporary management of hemorrhage after minimally invasive radical prostatectomy. Urology. 2019;130:120-125.
doi pubmed pmc - Pariser JJ, Pearce SM, Patel SG, Bales GT. National trends of simple prostatectomy for benign prostatic hyperplasia with an analysis of risk factors for adverse perioperative outcomes. Urology. 2015;86(4):721-725.
doi pubmed - Suer E, Gokce I, Yaman O, et al. Open prostatectomy is still a valid option for large prostates: a high-volume, single-center experience. Urology. 2008;72(1):90-94
- Alemozaffar M, Sanda M, Yecies D, Mucci LA, Stampfer MJ, Kenfield SA. Benchmarks for operative outcomes of robotic and open radical prostatectomy: results from the Health Professionals Follow-up Study. Eur Urol. 2015;67(3):432-438.
doi pubmed pmc - Manfredi M, Fiori C, Peretti D, Piramide F, Checcucci E, Garrou D, Amparore D, et al. Laparoscopic simple prostatectomy: complications and functional results after five years of follow-up. Minerva Urol Nefrol. 2020;72(4):498-504.
doi pubmed - Haapiainen H, Kaipia A, Murtola T, Seikkula H, Seppanen M, Jamsa P, Raitanen M. 3D laparoscopic prostatectomy: results of multicentre study. Scand J Urol. 2022;56(3):176-181.
doi pubmed - Porcaro AB, Siracusano S, Bizzotto L, Sebben M, Cacciamani GE, de Luyk N, Corsi P, et al. Is a drain needed after robotic radical prostatectomy with or without pelvic lymph node dissection? Results of a single-center randomized clinical trial. J Endourol. 2021;35(6):922-928.
doi pubmed - Chesnut GT, Benfante N, Barham D, Dean LW, Tin A, Sjoberg DD, Scardino PT, et al. Routine postoperative hemoglobin assessment poorly predictstransfusion requirement among patients undergoing minimally invasive radical prostatectomy. Urol Pract. 2020;7(4):299-304.
doi pubmed pmc - Health expenditure and financing: Health expenditure indicators (Edition 2021) (Internet), OECD Health Statistics (database). Cited on Sep 17, 2022. Available from: https://data.oecd.org/healthres/health-spending.htm.
- Nathan A, Hanna N, Rashid A, Patel S, Phuah Y, Flora K, Fricker M, et al. New recommendations to reduce unnecessary blood tests after robot-assisted radical prostatectomy. BJU Int. 2021;128(6):681-684.
doi pubmed - Berger AK, Chopra S, Desai MM, Aron M, Gill IS. Outpatient robotic radical prostatectomy: matched-pair comparison with inpatient surgery. J Endourol. 2016;30(Suppl 1):S52-56.
doi pubmed - Low AW, Chen K, Tan YG, Ng TK, Yuen JSP. Ambulatory robot-assisted laparoscopic radical prostatectomy with extended recovery by total extraperitoneal approach. Int J Urol. 2021;28(5):561-565.
doi pubmed - Abaza R, Martinez O, Ferroni MC, Bsatee A, Gerhard RS. Same day discharge after robotic radical prostatectomy. J Urol. 2019;202(5):959-963.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
